Complete Guide to BCL11A Enhancer Editing: Protocol for Exa-cel (exagamglogene autotemcel) Development and Optimization
This comprehensive guide details the protocol for editing the BCL11A enhancer region to produce exagamglogene autotemcel (exa-cel), an autologous CRISPR-Cas9 edited cell therapy for sickle cell disease and beta-thalassemia.
Complete Guide to BCL11A Enhancer Editing: Protocol for Exa-cel (exagamglogene autotemcel) Development and Optimization
Abstract
This comprehensive guide details the protocol for editing the BCL11A enhancer region to produce exagamglogene autotemcel (exa-cel), an autologous CRISPR-Cas9 edited cell therapy for sickle cell disease and beta-thalassemia. It explores the foundational science of the γ-globin repressor BCL11A, provides a step-by-step methodological workflow from patient apheresis to final drug product formulation, addresses critical troubleshooting and process optimization challenges, and validates the approach through comparative analysis with other curative strategies. Tailored for researchers and drug development professionals, this article synthesizes current clinical evidence, technical specifications, and future directions for this transformative genome editing therapy.
The Science of BCL11A: Unlocking Fetal Hemoglobin for Genetic Cure
Exagamglogene autotemcel (exa-cel), formerly known as CTX001, is an investigational, autologous ex vivo CRISPR/Cas9 genome-edited cell therapy for the treatment of sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TDT). Its therapeutic rationale is based on the precise disruption of an erythroid-specific enhancer of the BCL11A gene in a patient's own hematopoietic stem and progenitor cells (HSPCs). BCL11A is a transcriptional repressor of fetal hemoglobin (HbF, α2γ2). By reducing BCL11A expression in erythroid-lineage cells, exa-cel reactivates HbF production, which compensates for the deficient or dysfunctional adult hemoglobin (HbA) in TDT and SCD. The non-homologous end joining (NHEJ) repair of the CRISPR/Cas9-induced double-strand break in the enhancer region results in indels that disrupt the BCL11A binding motif, leading to sustained, high levels of HbF and consequent resolution of disease symptoms.
Application Notes and Protocols
Protocol forBCL11AEnhancer Editing in CD34+ HSPCs
Objective: To isolate, edit, and expand human CD34+ HSPCs for the generation of exagamglogene autotemcel product.
Materials:
- Human mobilized peripheral blood or bone marrow aspirate.
- CD34+ cell isolation kit (e.g., immunomagnetic beads).
- Serum-free expansion medium (SFEM) with cytokines (SCF, TPO, FLT3-L).
- CRISPR/Cas9 ribonucleoprotein (RNP) complex: recombinant S.p. Cas9 protein and synthetic sgRNA targeting the BCL11A erythroid-specific enhancer (e.g., within the GATA1 binding motif).
- Electroporation system (e.g., Lonza 4D-Nucleofector).
- In vitro erythroid differentiation media.
Method:
- CD34+ Cell Isolation: Isolate CD34+ HSPCs from leukapheresis product using positive immunomagnetic selection per manufacturer's protocol. Assess viability and purity via flow cytometry.
- Pre-stimulation: Culture cells in SFEM with cytokines (100 ng/mL SCF, 100 ng/mL TPO, 100 ng/mL FLT3-L) for 24-48 hours.
- RNP Electroporation: Form RNP complex by incubating Cas9 protein (60 pmol) with sgRNA (120 pmol) at room temperature for 10 minutes. Resuspend 1x10^6 pre-stimulated CD34+ cells in 100 µL electroporation buffer. Combine with RNP complex and electroporate using a pre-optimized program (e.g., EH-100 on 4D-Nucleofector). Include a non-edited control.
- Post-Electroporation Recovery: Immediately transfer cells to pre-warmed culture medium with cytokines. Culture at 37°C, 5% CO2.
- Quality Control and Expansion: Sample cells 48-72h post-electroporation for assessment of editing efficiency (via next-generation sequencing of the target locus). Expand edited cells in culture for 7-14 days.
- In Vitro Differentiation: For functional analysis, differentiate a portion of edited cells down the erythroid lineage in stage-specific media for 21 days. Analyze HbF expression via HPLC or flow cytometry.
Protocol for Assessing Editing Outcomes and HbF Reactivation
Objective: To quantify indels at the BCL11A enhancer and measure resultant fetal hemoglobin production.
Materials:
- Genomic DNA extraction kit.
- PCR primers flanking the BCL11A enhancer target site.
- Next-generation sequencing (NGS) library prep kit.
- HPLC system for hemoglobin analysis or anti-HbF antibodies for flow cytometry.
Method:
- Genomic DNA Extraction: Extract gDNA from edited and control cells at day 5-7 post-electroporation.
- Target Amplification: Amplify the target region by PCR (primers: F-5'-...-3', R-5'-...-3').
- NGS Analysis: Prepare NGS libraries and sequence on a MiSeq system. Analyze sequencing data using CRISPR-specific variant callers (e.g., CRISPResso2) to determine indel spectrum and frequency.
- HbF Quantification:
- HPLC: Lysate erythroid cells from day 21 of differentiation. Analyze lysate on a HPLC system configured for hemoglobin variant separation. Calculate % HbF of total hemoglobin.
- Flow Cytometry: Fix and permeabilize erythroid cells, stain with anti-HbF antibody conjugated to a fluorophore, and analyze on a flow cytometer. Report % HbF-positive cells and HbF content per cell (Mean Fluorescence Intensity).
Data Presentation
Table 1: Summary of Key Clinical Outcomes from exa-cel Trials
| Parameter | Sickle Cell Disease (Phase 3) | Transfusion-Dependent Beta Thalassemia (Phase 3) |
|---|---|---|
| Patients (n) | ~30 | ~50 |
| Follow-up (months) | Up to 36 | Up to 42 |
| VOC-Free (SCD) / Transfusion-Free (TDT) | ~96% (29/30) patients free of vaso-occlusive crises for ≥12 months post-infusion | ~93% (39/42) patients achieved transfusion independence for ≥12 months |
| Mean HbF Level | ~40% of total hemoglobin | >60% of total hemoglobin |
| Mean HbF per F-cell (pg) | ~10-12 pg/cell | ~10-12 pg/cell |
| Engraftment (Neutrophils) | Median time to neutrophil engraftment: ~27 days | Median time to neutrophil engraftment: ~28 days |
| Engraftment (Platelets) | Median time to platelet engraftment: ~37 days | Median time to platelet engraftment: ~36 days |
Table 2: Key Research Reagent Solutions for exa-cel Protocol Development
| Reagent/Material | Function/Explanation |
|---|---|
| CD34 MicroBead Kit | Immunomagnetic positive selection for human hematopoietic stem and progenitor cells from apheresis product. |
| Recombinant S.p. Cas9 Protein | High-purity, endotoxin-free Cas9 nuclease for formation of RNP complex; reduces off-target risk vs. plasmid DNA. |
| Chemically Modified sgRNA | Synthetic guide RNA with chemical modifications (e.g., 2'-O-methyl, phosphorothioate) to enhance stability and reduce immunogenicity. |
| X-VIVO 15 or StemSpan SFEM | Serum-free, defined media for the culture and expansion of HSPCs, ensuring consistency and regulatory compliance. |
| Cytokine Cocktail (SCF, TPO, FLT3-L) | Essential for maintaining stemness and promoting proliferation of HSPCs during pre-stimulation and post-editing culture. |
| 4D-Nucleofector System & P3 Kit | Optimized hardware and reagents for high-efficiency, low-toxicity delivery of RNP complexes into sensitive CD34+ cells. |
| Anti-HbF-PE Antibody | For flow cytometric detection and quantification of fetal hemoglobin in terminally differentiated erythroid cells. |
Visualizations
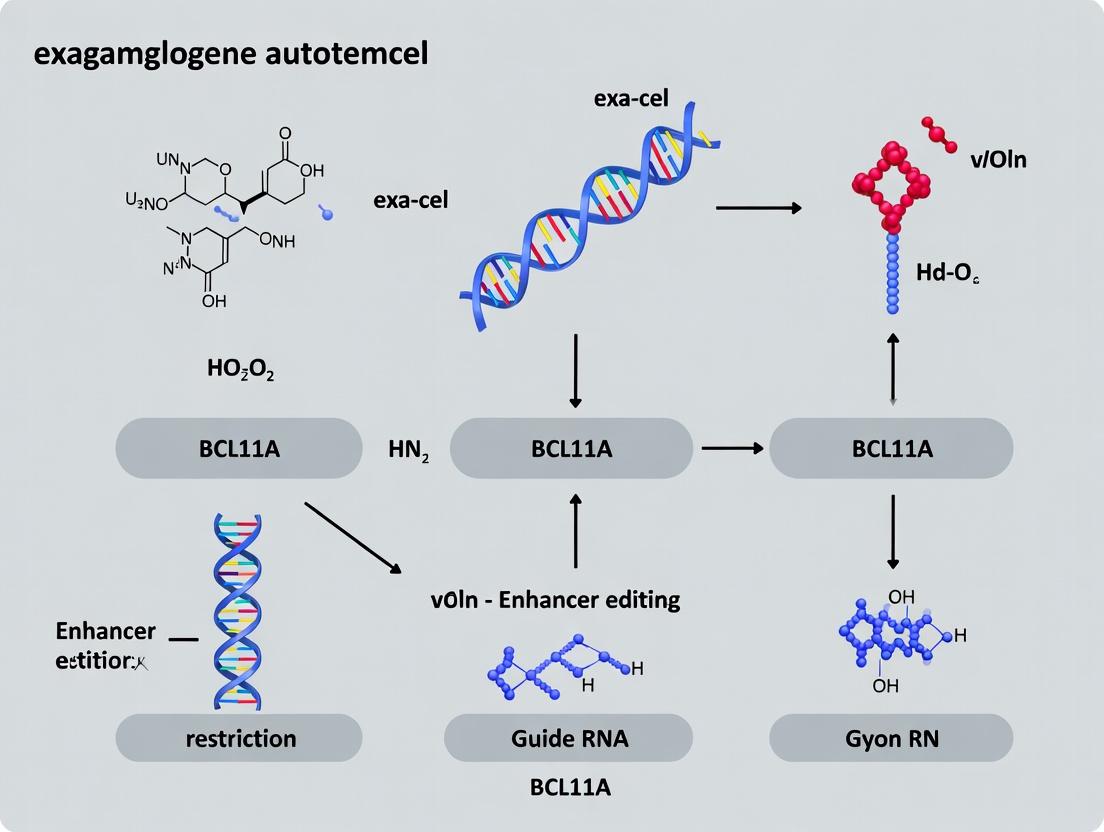
Title: Exa-cel Manufacturing and Treatment Workflow
Title: Molecular Mechanism of BCL11A Enhancer Editing
The Role of BCL11A as a Master Repressor of Fetal Hemoglobin (HbF).
Application Notes
Thesis Context: This document details methodologies central to the research underpinning the development of exagamglogene autotemcel (exa-cel), a CRISPR/Cas9-based gene therapy for sickle cell disease (SCD) and β-thalassemia. The therapeutic principle involves disrupting a specific enhancer within the BCL11A gene to reduce expression of the BCL11A protein, thereby de-repressing fetal hemoglobin (HbF, α2γ2) synthesis in adult red blood cells. Elevated HbF compensates for defective or absent adult hemoglobin (HbA, α2β2), alleviating disease pathophysiology.
Key Quantitative Summary:
Table 1: Clinical & Pre-Clinical Outcomes of BCL11A Targeting
| Parameter | Exa-cel Clinical Trial Data (Approx.) | In Vitro/Pre-Clinical Benchmark |
|---|---|---|
| Indel Frequency at Target | >90% in edited CD34+ cells | 70-95% (varies with guide, delivery) |
| HbF Increase | >40% of total Hb in responders | 20-40% F-cells in erythroid diffs |
| BCL11A Protein Downregulation | ~70-80% reduction in erythroid progeny | 50-90% reduction (Western Blot) |
| Transfusion Independence (SCD) | >90% of patients (up to 38 months) | N/A |
| VOC Resolution (SCD) | >90% of patients (up to 38 months) | N/A |
Table 2: Key Genomic Targets for HbF Reactivation
| Target Locus | Target Type | Editing Strategy | Primary Outcome |
|---|---|---|---|
| BCL11A Erythroid Enhancer (+58, +62, +63) | Non-coding, erythroid-specific | CRISPR/Cas9 disruption | Reduced BCL11A transcription specifically in erythroid lineage. |
| BCL11A Exon 2 | Coding region | CRISPR/Cas9 disruption | Frameshift mutation, complete loss of functional BCL11A protein. |
| γ-globin gene promoters | Promoter | CRISPR/dCas9-VP64 fusions (activation) | Direct transcriptional activation of HBG1/HBG2 genes. |
Experimental Protocols
Protocol 1: In Vitro Erythroid Differentiation and HbF Quantification via FACS
Purpose: To assess the functional consequence of BCL11A enhancer editing on HbF protein expression at the single-cell level.
Workflow:
- CD34+ Cell Culture: Isolate human hematopoietic stem and progenitor cells (HSPCs, CD34+) from mobilized peripheral blood or cord blood.
- Electroporation: Deliver CRISPR/Cas9 RNP (e.g., SpCas9 protein + sgRNA targeting the BCL11A +58 enhancer) via nucleofection.
- Erythroid Differentiation: Culture edited HSPCs in a three-phase erythroid differentiation medium (containing SCF, EPO, IL-3, dexamethasone, estradiol, etc.) over 18-21 days.
- Cell Staining: On day 18, harvest cells, fix, and permeabilize. Stain intracellularly with fluorescently conjugated antibodies against HbF (FITC) and the erythroid marker Glycophorin A (CD235a, PE).
- Flow Cytometry: Acquire data on a flow cytometer. Gate on viable, CD235a+ erythroid cells. The percentage of CD235a+ cells that are also HbF+ defines the "F-cell" population.
Protocol 2: Assessment of Editing Efficiency and Specificity (NGS)
Purpose: To quantify on-target modification and screen for potential off-target editing events.
Workflow:
- Genomic DNA Extraction: Isolate gDNA from edited and control cell populations (e.g., post-electroporation day 3 HSPCs or day 18 erythroid cells) using a column-based kit.
- On-target PCR Amplification: Design primers flanking the BCL11A enhancer target site (~300-400bp amplicon). Perform PCR using high-fidelity polymerase.
- Off-target Site Selection & Amplification: Identify potential off-target sites using algorithms (e.g., Cas-OFFinder). Amplify the top 10-20 predicted sites.
- Next-Generation Sequencing Library Prep: Purify PCR products and prepare sequencing libraries using a barcoding kit (e.g., Illumina). Pool samples.
- Sequencing & Analysis: Perform deep sequencing (MiSeq, NextSeq). Analyze reads for insertion/deletion (indel) patterns at the on-target locus. For off-targets, align reads to reference sequences to detect any mutations above background (e.g., >0.1%).
Protocol 3: BCL11A Expression Analysis via qRT-PCR and Western Blot
Purpose: To measure the transcriptional and translational knockdown of BCL11A resulting from enhancer disruption.
Workflow for qRT-PCR:
- RNA Extraction: Isolate total RNA from erythroid cells at differentiation days 10-14, when BCL11A expression peaks.
- cDNA Synthesis: Perform reverse transcription using random hexamers.
- Quantitative PCR: Run reactions with TaqMan probes or SYBR Green specific for BCL11A (all isoforms or erythroid-specific) and housekeeping genes (GAPDH, HPRT1).
- Analysis: Calculate ΔΔCt values to determine relative BCL11A mRNA expression in edited vs. control cells.
Workflow for Western Blot:
- Protein Lysate Preparation: Harvest erythroid cells (day 10-14), lyse in RIPA buffer with protease inhibitors.
- Electrophoresis & Transfer: Separate proteins by SDS-PAGE, transfer to PVDF membrane.
- Immunoblotting: Block membrane, incubate with primary antibodies (anti-BCL11A XL isoform, anti-β-actin loading control), then HRP-conjugated secondary antibodies.
- Detection: Use chemiluminescent substrate and imager. Quantify band intensity to determine BCL11A protein reduction.
Visualizations
Diagram 1: BCL11A-Mediated HbF Repression Logic
Diagram 2: Exa-cel Therapeutic Process Flow
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function / Application |
|---|---|
| CRISPR/Cas9 RNP Complex | Ribonucleoprotein of SpCas9 protein and synthetic sgRNA; direct delivery minimizes DNA vector exposure, increases editing speed and reduces off-target risk. |
| Human CD34+ HSPCs | Primary target cells for editing; sourced from mobilized peripheral blood, cord blood, or inducible pluripotent stem cells (iPSCs). |
| Erythroid Differentiation Media Kit (e.g., STEMdiff) | Serum-free, cytokine-defined medium for synchronized, high-yield production of enucleated erythroid cells from HSPCs. |
| Anti-HbF-FITC / Anti-CD235a-PE Antibodies | Essential pair for flow cytometric identification and quantification of HbF-expressing erythroid cells (F-cells). |
| BCL11A (D5C8F) Rabbit mAb | Validated antibody for detecting the BCL11A XL isoform by Western Blot in human erythroid lysates. |
| NGS-based Off-target Analysis Kit | Comprehensive system for amplifying, sequencing, and analyzing predicted off-target loci to assess editing specificity. |
| G-CSF / Plerixafor | Used for mobilizing HSPCs from bone marrow to peripheral blood for patient apheresis collection. |
| Busulfan | Myeloablative conditioning agent; clears bone marrow niches to enable engraftment of edited HSPCs. |
This protocol details the precise identification and validation of the CRISPR-Cas9 target site within the BCL11A erythroid enhancer, a critical step in the development of exagamglogene autotemcel (exa-cel). Within the broader thesis on enhancer editing protocols, this document establishes the foundational experimental workflow for site-specific disruption of the +58 DNase I hypersensitive site (DHS) within the BCL11A gene's intronic enhancer. This disruption is designed to reduce BCL11A expression in erythroid cells, thereby inducing fetal hemoglobin (HbF) production—the therapeutic mechanism for treating β-hemoglobinopathies like sickle cell disease and β-thalassemia.
Table 1: Key Genomic Coordinates of the BCL11A Erythroid Enhancer (GRCh38/hg38)
| Genomic Element | Chromosome | Start Position | End Position | Key Feature |
|---|---|---|---|---|
| BCL11A Gene | 2 | 60,709,843 | 60,888,113 | Encodes transcription factor |
| Erythroid Enhancer (+58 DHS) | 2 | 60,724,657 | 60,726,017 | Critical regulatory region |
| Prototype Target Site | 2 | 60,725,668 | 60,725,690 | sgRNA binding sequence |
Table 2: Efficacy Metrics from Pre-Clinical Studies (Representative Data)
| Experimental Model | Editing Efficiency (%) | HbF Induction (% of total Hb) | BCL11A Reduction (mRNA, %) |
|---|---|---|---|
| Human CD34+ HSCs in vitro | 75-90 | 20-40 | 70-85 |
| Mouse Xenograft Model | 60-80 | 25-45 | 65-80 |
| Clinical Trial (exa-cel) | ~90 (allelic editing) | >20 (patients) | 70-80 (erythroid progeny) |
Detailed Experimental Protocol for Target Site Identification & Validation
Protocol 3.1:In SilicoIdentification and sgRNA Design
Objective: To computationally identify optimal CRISPR-Cas9 target sequences within the +58 DHS region.
- Retrieve Genomic Sequence: Access the BCL11A locus (Chr2:60,724,657-60,726,017) from the UCSC Genome Browser (GRCh38/hg38 assembly).
- Identify Protospacer Adjacent Motif (PAM) Sites: Scan the sequence for all instances of the SpCas9 PAM sequence (5'-NGG-3').
- Select Candidate sgRNAs: For each PAM, extract the 20-nt upstream sequence as a potential sgRNA spacer. Prioritize sequences with:
- High on-target efficiency scores (using tools like Chop-Chop or CRISPOR).
- Minimal off-target potential (assess via genome-wide mismatch tolerance scanning).
- Location centered within the functional core of the +58 DHS (as defined by chromatin accessibility and transcription factor occupancy data).
- Final Selection: The lead target sequence for clinical development is: 5'-GCCAATCTGACTCCTAAGCC-3' (reverse strand, targeting the GATA1 motif region).
Protocol 3.2:In VitroValidation of Cutting Efficiency
Objective: To experimentally validate the cleavage efficiency of the designed sgRNA. Materials: See "Research Reagent Solutions" (Section 6). Method:
- Synthesize & Clone: Synthesize the sgRNA oligo and clone into the chosen CRISPR expression vector (e.g., pSpCas9(BB)-2A-GFP).
- Cell Transfection: Co-transfect HEK293T cells with the sgRNA/Cas9 plasmid and a plasmid containing a ~500-bp PCR-amplified genomic fragment encompassing the target site.
- Harvest DNA: Isolate genomic DNA from transfected cells 72 hours post-transfection.
- T7 Endonuclease I (T7EI) Assay: a. PCR-amplify the target locus from the isolated genomic DNA. b. Denature and re-anneal the PCR products to form heteroduplexes if indels are present. c. Digest with T7EI, which cleaves mismatched DNA. d. Analyze fragments by agarose gel electrophoresis. Calculate indel frequency using band intensity.
Protocol 3.3: Functional Validation in Primary Human CD34+ HSPCs
Objective: To confirm enhancer disruption, BCL11A downregulation, and HbF induction. Method:
- Electroporation: Deliver ribonucleoprotein (RNP) complexes of recombinant SpCas9 protein and synthetic sgRNA into mobilized human CD34+ hematopoietic stem and progenitor cells (HSPCs).
- Differentiation: Culture edited HSPCs in a three-phase erythroid differentiation medium for 18-21 days.
- Analysis:
- Genotyping: Perform Sanger sequencing of the target region from day 3 post-electroporation. Analyze indel spectra and frequency using TIDE or ICE analysis.
- Flow Cytometry: Quantify HbF protein expression in terminally differentiated erythroid cells (day 18) using intracellular staining with anti-HbF antibodies.
- qPCR: Measure BCL11A mRNA levels at the erythroid progenitor stage (day 10-12).
Visualization Diagrams
Experimental Workflow for Target Site Validation
Diagram 1: BCL11A Enhancer Target Site Validation Workflow
Mechanism of Action: Enhancer Disruption to HbF Induction
Diagram 2: From Enhancer Editing to Therapeutic HbF Induction
Research Reagent Solutions
Table 3: Essential Reagents for BCL11A Enhancer Target Site Experiments
| Reagent | Function/Description | Example Product/Catalog |
|---|---|---|
| Human CD34+ HSPCs | Primary cells for functional validation; source for ex vivo editing. | Mobilized peripheral blood-derived, human. |
| SpCas9 Nuclease (Recombinant) | High-purity protein for RNP complex formation, ensuring rapid activity and clearance. | TruCut HiFi Cas9 Protein or equivalent. |
| Chemically Modified sgRNA | Synthetic guide RNA with enhanced stability and reduced immunogenicity. | Synthego CRISPR guide, 2'-O-methyl 3' phosphorothioate modifications. |
| Electroporation System | For efficient delivery of RNP complexes into sensitive HSPCs. | Lonza 4D-Nucleofector, using P3 Primary Cell Kit. |
| Erythroid Differentiation Media | Serum-free, cytokine-defined medium to support red blood cell development from HSPCs. | STEMdiff Erythroid Expansion Kit or in-house formulation (EPO, SCF, IL-3, etc.). |
| Anti-HbF Antibody (FITC) | For detection and quantification of HbF protein in differentiated erythroblasts via flow cytometry. | BD Biosciences, clone HB-1 (FITC). |
| T7 Endonuclease I | Enzyme for detecting CRISPR-induced indels via mismatch cleavage assay. | NEB, M0302S. |
| BCL11A TaqMan Gene Expression Assay | For precise quantification of BCL11A mRNA knockdown in edited cells. | Thermo Fisher Scientific, Hs00232723_m1. |
Sickle Cell Disease (SCD) and transfusion-dependent Beta-Thalassemia (TDT) are monogenic hemoglobinopathies arising from mutations in the β-globin gene (HBB). In SCD, a point mutation (GAG→GTG) leads to the production of abnormal hemoglobin S (HbS), which polymerizes under deoxygenation, causing sickling of red blood cells (RBCs), chronic hemolysis, vaso-occlusion, and multi-organ damage. In TDT, mutations cause reduced or absent β-globin synthesis, leading to severe anemia, ineffective erythropoiesis, and iron overload.
Both diseases share a pathophysiological hallmark: an imbalance in the globin chains that make up hemoglobin. A key compensatory mechanism is the continued postnatal expression of fetal hemoglobin (HbF, α2γ2), which is naturally silenced after birth by transcriptional regulators like BCL11A. HbF is an effective anti-sickling agent and can compensate for deficient β-globin in thalassemia. Therefore, the therapeutic reactivation of HbF via disruption of the BCL11A gene or its erythroid-specific enhancer represents a powerful one-time curative strategy. This application note focuses on the protocol for exagamglogene autotemcel (exa-cel), a CRISPR-Cas9-based therapy that edits the BCL11A enhancer in autologous hematopoietic stem and progenitor cells (HSPCs).
Table 1: Comparative Pathophysiology of SCD and TDT
| Parameter | Sickle Cell Disease (SCD) | Transfusion-Dependent β-Thalassemia (TDT) |
|---|---|---|
| Genetic Defect | Single nucleotide variant in HBB (HbS) | >200 variants causing reduced/absent β-globin |
| Primary Hb | HbS (α2βS2) | HbA (α2β2) severely deficient |
| Pathogenic Trigger | Deoxygenation | Imbalanced α/β-globin chain ratio |
| Key Pathology | HbS polymerization, sickling, hemolysis, vaso-occlusion | Ineffective erythropoiesis, hemolysis, iron overload |
| Therapeutic HbF Target | >20-30% HbF, >7-9 pg HbF/RBC (anti-sickling threshold) | Total Hb sufficient to eliminate transfusion need (≥9 g/dL) |
Table 2: Clinical Outcomes from Pivotal exa-cel Trials (CLIMB-111 & CLIMB-121)
| Outcome Measure | SCD Patients (N=~30) | TDT Patients (N=~40) |
|---|---|---|
| Freedom from Severe VOCs (≥12 mo) | ~96% (24/25 evaluable) | Not Applicable |
| Transfusion Independence (≥12 mo) | Not Applicable | ~93% (39/42 evaluable) |
| Mean HbF Percentage (Month 24) | ~40% | ~60% |
| Mean Total Hemoglobin (Month 24) | ~12 g/dL | ~13 g/dL |
| Common AEs (Post-Infusion) | Neutropenia, Thrombocytopenia, Mucositis, Febrile Neutropenia |
Research Reagent Solutions Toolkit
Table 3: Essential Materials for BCL11A Enhancer Editing Protocols
| Reagent/Material | Function/Explanation |
|---|---|
| G-CSF & Plerixafor | Mobilizing agents for collection of peripheral blood CD34+ HSPCs. |
| CliniMACS CD34 Reagent System | Clinical-grade magnetic separation for positive selection of CD34+ cells. |
| CRISPR-Cas9 RNP Complex | Pre-complexed, synthetic guide RNA (sgRNA targeting BCL11A enhancer) and Cas9 protein. Enables precise, transient editing. |
| Electroporation System (e.g., MaxCyte GTx) | Clinically scalable electroporator for efficient, non-viral delivery of RNP into HSPCs. |
| StemSpan SFEM II Medium | Serum-free, cytokine-supplemented medium for culturing HSPCs during and post-editing. |
| Myeloablative Busulfan | Conditioning regimen to create marrow niche for engraftment of edited HSPCs. |
| qPCR/ddPCR Assays | For measuring on-target editing efficiency, vector copy number, and myeloid enrichment. |
| HPLC/Capillary Electrophoresis | For quantification of HbF (%) at the protein level. |
| Next-Generation Sequencing (NGS) | For comprehensive analysis of on-target edits and off-target screening. |
Detailed Experimental Protocol: Exagamglogene Autotemcel Manufacturing
Protocol Title: Clinical-Scale Manufacturing of BCL11A-Enhancer Edited CD34+ HSPCs (exa-cel)
Objective: To genetically modify autologous CD34+ HSPCs via CRISPR-Cas9 editing of the +58 BCL11A erythroid-specific enhancer region to induce HbF expression.
Materials:
- Mobilized leukapheresis product from patient.
- CliniMACS PBS/EDTA buffer, CliniMACS CD34 Reagent.
- Buffer for electroporation (MaxCyte Electroporation Buffer).
- Synthetic sgRNA (sequence: 5'-GGCAGAAGCCGCACAGCATG-3') and Cas9 protein.
- MaxCyte GTx Electroporation System.
- StemSpan SFEM II medium with cytokines (SCF, TPO, FLT3-L).
- QC assays: Flow cytometry (CD34+ viability), ddPCR (editing %), CFU assays.
Methodology:
CD34+ Cell Isolation:
- Process leukapheresis product within 24h.
- Isolate CD34+ HSPCs using the CliniMACS Prodigy system with clinical-grade CD34 microbeads.
- Perform cell count and viability assessment (target: ≥90% viability).
CRISPR-Cas9 RNP Complex Formation:
- Thaw and resuspend sgRNA and Cas9 protein in nuclease-free buffer.
- Pre-complex the RNP by mixing sgRNA and Cas9 protein at a molar ratio of 2:1 (sgRNA:Cas9). Incubate at room temperature for 10 minutes.
Electroporation:
- Wash isolated CD34+ cells and resuspend in electroporation buffer at a concentration of 1.0 x 10^8 cells/mL.
- Mix cells with pre-complexed RNP (final sgRNA concentration: 60 µM).
- Transfer cell/RNP mixture to an OC-400 processing assembly.
- Electroporate using the MaxCyte GTx "CL-4" pre-optimized protocol.
- Immediately post-electroporation, transfer cells to pre-warmed StemSpan medium with cytokines.
Post-Editing Culture & QC Release:
- Culture edited cells for 1-2 days in a 37°C, 5% CO2 incubator.
- Quality Control Testing: a. Viability & Recovery: Flow cytometry with 7-AAD/CD34. b. Editing Efficiency: ddPCR assay quantifying INDEL frequency at the BCL11A enhancer target site (release spec: >70%). c. Potency: Colony-forming unit (CFU) assay and HbF induction in erythroid differentiation cultures. d. Safety: Sterility, mycoplasma, and endotoxin testing. NGS-based off-target analysis on a representative aliquot.
Cryopreservation & Infusion:
- Cryopreserve the final drug product (edited CD34+ cells) in CryoStor CS10.
- The patient undergoes myeloablative conditioning with busulfan.
- Thaw drug product at bedside and infuse intravenously.
Signaling Pathways and Workflow Visualizations
Table 1: Key In Vitro and In Vivo Efficacy Data from BCL11A Enhancer Targeting Studies
| Model System | Intervention | Key Metric | Result (Mean ± SD or %) | Reference/Study |
|---|---|---|---|---|
| Human CD34+ HSPCs (Sickle Cell Disease genotype) | CRISPR-Cas9 disruption of BCL11A erythroid enhancer | Fetal Hemoglobin (HbF) induction | 25-30% HbF+ cells (Baseline: <5%) | Canver et al., Nature, 2015 |
| Indel frequency at on-target site | ~80% | Canver et al., Nature, 2015 | ||
| Humanized mouse model (SCD) | Transplant of edited SCD HSPCs | HbF per red cell (F-cells) | >60% F-cells at 16 weeks | Wu et al., Science Translational Medicine, 2019 |
| Pathological improvement | Near-complete correction of sickling, normalized RBC half-life | Wu et al., Science Translational Medicine, 2019 | ||
| Non-human primate (NHP) model | Transplant of CRISPR-edited HSPCs (targeting BCL11A enhancer) | Long-term engraftment | >20% editing persistence in myeloid/lymphoid cells at 1 year | Pre-clinical data for exa-cel |
| Safety profile | No evidence of genotoxicity or clonal dominance | Pre-clinical data for exa-cel |
Table 2: Specificity & Off-target Analysis (Representative Data)
| Analysis Method | Target Site | Findings | Implication |
|---|---|---|---|
| In silico prediction (Cas-OFFinder) | BCL11A +58kb enhancer | Top 10 predicted off-targets with 3-4 mismatches | Guide selection for low predicted off-target risk |
| CIRCLE-seq / GUIDE-seq | Genomic DNA from edited cells | No detectable off-target editing above assay background (<0.1%) | High specificity of the selected sgRNA |
| RNA-seq | Edited HSPCs vs. Control | No significant differential expression in genes near predicted off-targets | Confirmation of on-target specificity |
Detailed Experimental Protocols
Protocol 2.1: In Vitro Editing of Human CD34+ HSPCs and HbF Analysis
Objective: To disrupt the BCL11A erythroid enhancer in hematopoietic stem and progenitor cells (HSPCs) and quantify fetal hemoglobin (HbF) reactivation.
Materials: See Scientist's Toolkit (Section 4).
Procedure:
- CD34+ HSPC Isolation & Culture: Isolate CD34+ cells from mobilized peripheral blood or cord blood using immunomagnetic beads. Pre-stimulate cells for 48 hours in serum-free medium supplemented with SCF (100 ng/ml), TPO (100 ng/ml), FLT3-L (100 ng/ml).
- RNP Electroporation: Complex chemically modified sgRNA (targeting the +58 GATA1 motif) with recombinant high-fidelity SpCas9 protein to form ribonucleoprotein (RNP). Use a 2:1 molar ratio (sgRNA:Cas9). Electroporate 1x10^5 HSPCs using a Lonza 4D-Nucleofector (program DZ-100 or equivalent) with P3 buffer.
- Post-editing Culture: Immediately transfer cells to fresh, pre-warmed cytokine medium. Allow recovery for 24 hours.
- **Erythroid Differentiation: Transfer edited cells into erythroid differentiation medium (StemSpan with EPO (3 U/ml), SCF (50 ng/ml), IL-3 (5 ng/ml), dexamethasone (1µM), estradiol (1µM)). Culture for 14-16 days, diluting cells every 2-3 days.
- **Genotyping & Editing Efficiency:
- Harvest cells at day 3-4 post-electroporation for genomic DNA.
- PCR amplify the on-target region. Assess indel frequency via T7 Endonuclease I (T7EI) assay or next-generation sequencing (NGS).
- **HbF Quantification (Flow Cytometry): At day 14-16 of differentiation, fix and permeabilize erythroid cells. Stain intracellularly with FITC-conjugated anti-HbF antibody and PE-conjugated anti-HbA antibody. Analyze by flow cytometry. Gate on mature erythroid cells (CD235a+), and report the percentage of HbF-positive cells (F-cells).
Protocol 2.2: In Vivo Assessment in a Humanized Mouse Model of SCD
Objective: To evaluate the long-term engraftment, safety, and phenotypic correction of sickle cell disease by BCL11A enhancer-edited HSPCs.
Procedure:
- HSPC Editing & Transplant Preparation: Edit SCD patient-derived CD34+ HSPCs as in Protocol 2.1. Include a non-edited control from the same donor.
- Mouse Conditioning: Irradiate NSG or NSG-SGM3 mice (8-12 weeks old) with a sublethal dose (250-275 cGy) 24 hours prior to transplant.
- Transplantation: Inject 2-5 x 10^5 edited or control HSPCs via tail vein.
- Peripheral Blood Monitoring: Bleed mice monthly from the retro-orbital sinus. Assess:
- Human chimerism: Flow cytometry for hCD45+ cells.
- HbF production: Flow cytometry of red blood cells (Ter119+) for HbF staining.
- Sickling assay: Deoxygenate peripheral blood and assess percentage of sickled RBCs microscopically.
- Terminal Analysis (16-24 weeks): Sacrifice mice. Analyze bone marrow for:
- Multilineage engraftment: Flow cytometry for myeloid (hCD33+), lymphoid (hCD19+), and progenitor (hCD34+) human cells.
- Editing persistence: NGS on genomic DNA from sorted human cell populations.
- Progenitor function: Colony-forming unit (CFU) assays.
- Histopathology: Examine spleen, liver, and other organs for signs of extramedullary hematopoiesis or pathology.
Visualizations
Title: BCL11A Enhancer Targeting Logic for SCD
Title: Pre-clinical Workflow for BCL11A Enhancer Editing
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for BCL11A Enhancer Editing Experiments
| Reagent/Material | Supplier Examples | Function in Protocol |
|---|---|---|
| Human CD34+ HSPCs | Lonza, StemCell Technologies | Primary cell source for editing and functional assays. |
| Recombinant HiFi Cas9 Protein | Integrated DNA Technologies (IDT), Thermo Fisher | High-fidelity nuclease for precise cleavage with reduced off-target effects. |
| Chemically Modified sgRNA (targeting +58 site: e.g., 5'-GCCCACAGTGGCACCTGGGC-3') | Synthego, IDT | Guides Cas9 to the specific GATA1 motif within the BCL11A erythroid enhancer. Enhanced stability. |
| Nucleofector Kit & Device (4D-Nucleofector) | Lonza | Enables efficient, non-viral delivery of RNP complexes into hard-to-transfect HSPCs. |
| Erythroid Differentiation Media Kit | StemCell Technologies (StemSpan) | Provides optimized cytokines and supplements for robust in vitro erythroid differentiation from HSPCs. |
| Anti-Human HbF-FITC / HbA-PE Antibodies | BD Biosciences, Invitrogen | Critical for flow cytometric quantification of HbF reactivation at the single-cell level. |
| NGS-based Indel Analysis Kit (e.g., Illumina MiSeq) | Illumina, Paragon Genomics | Gold-standard for quantitative assessment of on-target editing efficiency and purity. |
| Immunodeficient Mouse Strains (NSG, NSG-SGM3) | The Jackson Laboratory | In vivo model for assessing long-term engraftment and functional correction of edited human HSPCs. |
Step-by-Step Protocol: Manufacturing Exa-cel from Apheresis to Infusion
Application Notes
This protocol details the critical initial stage of hematopoietic stem and progenitor cell (HSPC) collection for use in the exagamglogene autotemcel (exa-cel) manufacturing process. Exa-cel is an investigational autologous cell therapy for sickle cell disease and β-thalassemia that utilizes CRISPR-Cas9 to edit the erythroid-specific enhancer of BCL11A in patient HSPCs to induce fetal hemoglobin (HbF). The quality, quantity, and viability of the collected CD34+ HSPCs are the foundational determinants of the success of downstream genetic modification, manufacturing, and eventual therapeutic efficacy. This stage encompasses patient evaluation, mobilization of HSPCs from the bone marrow niche into the peripheral blood, and leukapheresis for collection.
Key Objectives:
- Safely mobilize a sufficient number of CD34+ HSPCs from the patient's bone marrow.
- Collect ≥ 6.0 x 10^6 CD34+ cells/kg of patient body weight via apheresis in a minimal number of sessions.
- Ensure cell product viability and purity to meet manufacturing release criteria.
- Minimize patient morbidity and manage potential side effects of mobilization.
Patient Population & Considerations: Patients must undergo comprehensive eligibility screening, including assessment of organ function, infectious disease status, and adequacy of venous access. For patients with sickle cell disease, special attention is paid to hydration, oxygenation, and pain management to prevent vaso-occlusive crises during mobilization and apheresis.
Detailed Protocol
Patient Mobilization
The goal is to increase the concentration of CD34+ HSPCs in the peripheral blood from a baseline of < 0.01% to a target of > 20 cells/μL.
Materials & Reagents:
- Granulocyte Colony-Stimulating Factor (G-CSF): Recombinant human G-CSF (e.g., Filgrastim). MOA: Binds to G-CSF receptors on neutrophils and bone marrow stromal cells, disrupting the CXCL12-CXCR4 axis and releasing HSPCs.
- Plerixafor (Mozobil): A CXCR4 chemokine receptor antagonist. MOA: Blocks binding of stromal cell-derived factor-1 (SDF-1/CXCL12) to CXCR4 on HSPCs, promoting their egress from the bone marrow.
- Supportive Medications: Prophylactic antibiotics, anti-pyretics (e.g., acetaminophen), and hydration fluids.
Methodology:
- G-CSF Priming: Administer Filgrastim subcutaneously at a dose of 10 μg/kg/day for 4-5 consecutive days.
- Plerixafor Boost: On the evening of Day 4 (approximately 10-12 hours prior to the planned first apheresis), administer Plerixafor subcutaneously at a dose of 0.24 mg/kg. This is critical for patients predicted to have poor mobilization (e.g., those with prior hydroxyurea use or splenic dysfunction).
- Monitoring: Monitor the patient daily for side effects (bone pain, fever, headache). Perform a complete blood count (CBC) daily. On the morning of Day 5, measure the peripheral blood CD34+ count via flow cytometry.
Decision Point: If the pre-apheresis CD34+ count is ≥ 20 cells/μL, proceed to leukapheresis. If < 20 cells/μL, consider an additional day of G-CSF and a second dose of Plerixafor.
Leukapheresis (HSPC Collection)
Materials & Equipment:
- Apheresis system (e.g., Spectra Optia, Fenwal Amicus).
- Continuous-flow cell separator kit.
- Anticoagulant (ACD-A).
- Calcium supplementation (oral or IV).
- Sterile collection bags.
Methodology:
- Venous Access: Establish adequate venous access, typically via bilateral peripheral antecubital veins. A temporary central venous catheter may be required if peripheral access is insufficient.
- Procedure Setup: Prime the apheresis system with anticoagulant. The typical blood processing volume is 2-3 times the patient's total blood volume, processed over 4-6 hours.
- Collection: The mononuclear cell (MNC) fraction containing the CD34+ HSPCs is collected into a sterile, single-use bag. The remainder of the blood components are returned to the patient.
- Patient Monitoring: Monitor for hypocalcemia symptoms (paresthesia, cramping) due to citrate anticoagulation and provide calcium supplements as needed. Monitor vital signs regularly.
- Post-Collection Handling: The apheresis product is immediately mixed with a cryoprotectant solution, typically containing DMSO and human serum albumin. It is then controlled-rate frozen and stored in the vapor phase of liquid nitrogen (< -150°C) until shipment to the manufacturing facility.
Product Testing & Release Criteria
The leukapheresis product must meet predefined specifications before being accepted for manufacturing.
Table 1: Key Acceptance Criteria for Leukapheresis Product
| Parameter | Target Specification | Analytical Method |
|---|---|---|
| Total Nucleated Cell (TNC) Count | Record and report | Automated cell counter |
| Total Viable CD34+ Cells | ≥ 6.0 x 10^6 cells/kg | Flow cytometry (ISHAGE gating) + 7-AAD |
| CD34+ Cell Viability | ≥ 80% | Flow cytometry (7-AAD or propidium iodide) |
| Cell Purity (CD34+ % of MNCs) | Report value | Flow cytometry |
| Sterility (Bacteria/Fungi) | No growth | BacT/ALERT microbial culture |
| Endotoxin | < 5.0 EU/kg | Limulus Amebocyte Lysate (LAL) assay |
| Gram Stain | Negative | Microscopy |
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for HSPC Mobilization & Analysis
| Item | Function/Application |
|---|---|
| Recombinant Human G-CSF (Filgrastim) | Mobilizing agent; disrupts HSPC retention in bone marrow. |
| Plerixafor (AMD3100) | CXCR4 antagonist; synergizes with G-CSF to enhance HSPC egress. |
| Anti-human CD34 Antibody (conjugated) | Primary reagent for enumeration and viability assessment of HSPCs via flow cytometry. |
| 7-Aminoactinomycin D (7-AAD) | DNA intercalating dye used as a viability stain for flow cytometry. |
| Lymphoprep or Ficoll-Paque | Density gradient medium for isolation of mononuclear cells from apheresis product if needed. |
| StemSpan SFEM II | Serum-free, cytokine-supplemented medium for ex vivo HSPC culture and functional assays. |
| MethoCult H4434 | Semi-solid methylcellulose medium for colony-forming unit (CFU) assays to assess HSPC functionality. |
| MycoAlert Detection Kit | Assay for detection of mycoplasma contamination in cell cultures. |
Pathway & Workflow Diagrams
Diagram 1: Patient mobilization and collection workflow.
Diagram 2: Molecular mechanisms of G-CSF and plerixafor mobilization.
This application note details a standardized protocol for ex vivo genome editing of the BCL11A erythroid enhancer in CD34+ hematopoietic stem and progenitor cells (HSPCs), forming the foundational manufacturing step for exagamglogene autotemcel (exa-cel). This process utilizes CRISPR-Cas9 ribonucleoprotein (RNP) electroporation to achieve high-efficiency on-target modification with minimized off-target risks.
Table 1: Critical Processing and Electroporation Parameters
| Parameter | Specification / Typical Value | Purpose/Rationale |
|---|---|---|
| Starting Material | Mobilized peripheral blood CD34+ cells (>90% purity, >90% viability) | Ensures high-quality, potent HSPCs for editing and engraftment. |
| Pre-Stimulation | 24-48 hours in serum-free medium with SCF, TPO, FLT3L | Primes cells for the cell cycle, enhancing electroporation efficiency. |
| CRISPR-Cas9 RNP | Cas9 nuclease: 60 µg/mL; sgRNA: 120 µg/mL (3:1 molar ratio) | Optimized for high editing efficiency while minimizing RNP-associated toxicity. |
| Electroporation Buffer | Proprietary, non-ionic, high-resistivity buffer | Reduces arcing and increases cell viability post-pulse. |
| Electroporation Device | 4D-Nucleofector (Lonza) | Industry-standard for reproducible HSPC transfection. |
| Pulse Code | EO-115 program | Specific waveform for CD34+ cells balancing delivery and survival. |
| Cell Density | 1-2 x 10^6 cells per 100 µL reaction | Optimal density for consistent nucleofection. |
| Post-Pulse Recovery | Immediate transfer to pre-warmed, cytokine-rich medium | Maximizes cell viability and supports DNA repair post-editing. |
| Target Editing Efficiency | 80-95% allele modification (INDELs + HDR) | Therapeutic threshold for sufficient fetal hemoglobin (HbF) induction. |
| Cell Viability (24h post-EP) | 50-70% | Expected range post-electroporation; cells recover in culture. |
Detailed Experimental Protocol
Protocol 2.1: Pre-Stimulation of CD34+ HSPCs
- Thawing: Rapidly thaw cryopreserved CD34+ cells in a 37°C water bath. Dilute dropwise in pre-warmed, complete serum-free medium (e.g., StemSpan SFEM II) containing 1% penicillin-streptomycin and 1U/mL DNase I.
- Wash: Centrifuge at 300 x g for 10 minutes. Aspirate supernatant and resuspend cell pellet gently.
- Culture: Seed cells at 0.5-1 x 10^6 cells/mL in pre-stimulation medium supplemented with recombinant human cytokines: Stem Cell Factor (SCF, 100 ng/mL), Thrombopoietin (TPO, 100 ng/mL), and FMS-like tyrosine kinase 3 ligand (Flt3L, 100 ng/mL).
- Incubate: Culture cells for 24-48 hours in a humidified incubator at 37°C, 5% CO₂.
Protocol 2.2: CRISPR-Cas9 RNP Complex Formation
- Reagent Preparation: Dilute high-fidelity S. pyogenes Cas9 protein and synthetic, chemically modified sgRNA (targeting the BCL11A +58 BCL11A binding site within the erythroid enhancer) in nuclease-free duplex buffer.
- Complexation: For a single reaction, combine 60 µg of Cas9 protein with 120 µg of sgRNA. Mix gently by pipetting.
- Incubation: Incubate the mixture at room temperature for 10-20 minutes to allow for complete RNP complex formation.
Protocol 2.3: Electroporation of HSPCs
- Cell Harvest: After pre-stimulation, collect cells and perform a viable cell count. Centrifuge at 300 x g for 10 minutes.
- Resuspension: Aspirate supernatant completely. Resuspend the cell pellet in the specified electroporation buffer at a density of 1-2 x 10^7 cells/mL.
- RNP Delivery: For each 100 µL electroporation sample, combine 10 µL of the prepared RNP complex with 90 µL of cell suspension. Mix gently and transfer the entire 100 µL to a certified electroporation cuvette.
- Pulse Application: Place the cuvette in the 4D-Nucleofector X unit and execute the pre-validated pulse code EO-115.
- Immediate Recovery: Immediately after pulsing, add 500 µL of pre-warmed (37°C) complete cytokine medium (as in Protocol 2.1) directly to the cuvette. Using the provided transfer pipette, gently resuspend and transfer the cells to a pre-warmed culture plate.
- Post-Electroporation Culture: Place cells in the incubator. For analytical assessments, sample cells at 48-72 hours post-electroporation for editing efficiency analysis (e.g., by next-generation sequencing or T7E1 assay).
Workflow and Pathway Diagrams
Title: Ex Vivo CRISPR Editing Workflow for HSPCs
Title: Molecular Outcome of BCL11A Enhancer Editing
The Scientist's Toolkit: Key Research Reagent Solutions
Table 2: Essential Materials and Reagents
| Item | Function/Explanation | Example/Supplier (Typical) |
|---|---|---|
| G-CSF Mobilized CD34+ Cells | The primary therapeutic starting material; source of human HSPCs. | Apheresis product from healthy donors. |
| Serum-Free Expansion Medium | Chemically defined, xeno-free medium for consistent HSPC culture. | StemSpan SFEM II (StemCell Technologies). |
| Recombinant Human Cytokines | Key signaling molecules for HSPC survival, priming, and proliferation. | SCF, TPO, Flt3L (PeproTech, CellGenix). |
| High-Fidelity Cas9 Nuclease | Engineered Cas9 protein with reduced off-target activity. | HiFi Cas9 (Integrated DNA Technologies) or similar. |
| Chemically Modified sgRNA | Synthetic guide RNA with enhanced stability and reduced immunogenicity. | Alt-R CRISPR-Cas9 sgRNA (IDT) with 2'-O-methyl analogs. |
| 4D-Nucleofector System | Optimized electroporation device for high-efficiency delivery into HSPCs. | Lonza. |
| P3 Primary Cell 4D-Nucleofector X Kit | Buffer and cuvette system specifically optimized for CD34+ HSPCs. | Lonza, Cat. No. V4XP-3024. |
| NGS Editing Analysis Kit | For quantitative, unbiased measurement of on- and off-target editing. | Illumina MiSeq with amplicon sequencing. |
| Donor Template (for HDR) | Single-stranded oligonucleotide (ssODN) or AAV6 vector containing desired homologies. | For precise enhancer edits or reporter integrations. |
1. Introduction and Thesis Context This document details Stage 3 of a comprehensive thesis protocol for developing exagamglogene autotemcel (exa-cel), an autologous CRISPR-Cas9-edited cell therapy for sickle cell disease and β-thalassemia. The therapeutic goal is to disrupt the erythroid-specific enhancer of BCL11A, a transcriptional repressor of fetal hemoglobin (HbF). This targeted disruption reduces BCL11A expression in erythroid lineage cells, thereby de-repressing HbF production, which can ameliorate disease symptoms. This stage focuses on the rational design and rigorous in vitro validation of single guide RNAs (sgRNAs) targeting the critical GATA1 motif within the +58 erythroid enhancer region of BCL11A.
2. Guide RNA (sgRNA) Design and Screening Strategy
2.1. Target Selection The target is a conserved GATA1 transcription factor binding site within the +58 DNase I hypersensitive site (HS2) of the BCL11A erythroid enhancer on chromosome 2. Disruption of this site is predicted to impair enhancer activity without affecting the BCL11A coding sequence.
Table 1: Candidate sgRNA Sequences Targeting the BCL11A +58 Enhancer Region
| sgRNA ID | Protospacer Sequence (5' to 3') | PAM | Genomic Coordinates (hg38) | Predicted On-Target Efficiency Score* | Predicted Off-Target Count (≤3 mismatches) |
|---|---|---|---|---|---|
| BCL11A-E1 | GGGGCCACTAGGGACAGGAT | AGG | chr2:60,750,102-60,750,121 | 68 | 12 |
| BCL11A-E2 | GATAAGAGTAACTGCCCGGC | TGG | chr2:60,750,087-60,750,106 | 72 | 8 |
| BCL11A-E3 | CCACTAGGGACAGGATGGGC | AGG | chr2:60,750,105-60,750,124 | 65 | 5 |
| BCL11A-E4 | AGAGTAACTGCCCGGCACCC | GGG | chr2:60,750,082-60,750,101 | 70 | 15 |
Efficiency scores (0-100 scale) from published algorithms (e.g., ChopChop, CRISPick). *In silico genome-wide search using reference genome GRCh38.
2.2. In silico Off-Target Analysis Protocol
- Tool: Use Cas-OFFinder or CRISPOR with default parameters.
- Input: Each candidate sgRNA protospacer sequence (20-nt).
- Parameters: Search genome (GRCh38), allow up to 3 nucleotide mismatches, include NGG PAM.
- Output: Generate a ranked list of potential off-target sites. Prioritize sites in coding exons, conserved non-coding regions, or known regulatory elements of other genes for subsequent evaluation.
3. Experimental Protocols for sgRNA Validation
3.1. Protocol: T7 Endonuclease I (T7E1) Assay for Initial Editing Efficiency
- Purpose: To rapidly assess the indel formation efficiency of candidate sgRNAs in bulk cell populations.
- Materials: sgRNA/Cas9 expression plasmids or RNP complexes, HEK293T or K562 cells, transfection reagent, genomic DNA extraction kit, PCR primers flanking target site, T7 Endonuclease I enzyme, agarose gel electrophoresis system.
- Procedure:
- Transfection/Electroporation: Deliver sgRNA:Cas9 ribonucleoprotein (RNP) complexes or plasmids into 2e5 cells per condition.
- Harvest: 72 hours post-delivery, extract genomic DNA.
- PCR Amplification: Amplify a ~500-800bp region surrounding the on-target site using high-fidelity polymerase.
- Heteroduplex Formation: Denature and reanneal PCR products (95°C for 10 min, ramp down to 25°C at -0.1°C/sec).
- Digestion: Incubate reannealed DNA with T7E1 enzyme at 37°C for 30 minutes.
- Analysis: Run products on a 2% agarose gel. Cleavage products indicate presence of indels. Calculate editing efficiency using band intensity analysis software.
3.2. Protocol: Next-Generation Sequencing (NGS) for Precise Editing Characterization
- Purpose: To quantify editing efficiency at single-nucleotide resolution and characterize the spectrum of induced insertions and deletions (indels).
- Materials: Purified genomic DNA from edited cells, target-specific PCR primers with Illumina adapter overhangs, high-fidelity PCR master mix, NGS cleanup beads, Illumina sequencing platform.
- Procedure:
- Library Preparation: Perform a two-step PCR. Step 1: Amplify target locus with barcoded primers. Step 2: Add full Illumina sequencing adapters and sample indices.
- Purification: Clean up PCR products using magnetic beads.
- Quantification & Pooling: Quantify libraries by qPCR, then pool equimolarly.
- Sequencing: Run on a MiSeq or comparable system (2x150bp or 2x250bp chemistry).
- Analysis: Process reads through a pipeline (e.g., CRISPResso2) to align sequences, quantify indels, and visualize mutation spectra.
Table 2: NGS Validation Results for Lead sgRNA (BCL11A-E2)
| Metric | Value in K562 Cells (RNP Delivery) | Value in CD34+ HSPCs (RNP Delivery) |
|---|---|---|
| Total Sequencing Depth | ~100,000x | ~50,000x |
| Alleles Modified (%) | 92.5% ± 3.1% | 85.7% ± 4.5% |
| Predominant Indel Type | -1bp deletion | -1bp deletion |
| Frequency of -1bp Deletion | 68.2% of modified alleles | 61.5% of modified alleles |
| Alleles with >5bp Deletion | 8.3% | 12.1% |
| Perfect HDR-Mediated Correction | N/A (Not applicable for knockout) | N/A |
3.3. Protocol: In Vitro Functional Validation via Erythroid Differentiation
- Purpose: To confirm that enhancer editing leads to reduced BCL11A expression and increased HbF production in a relevant cellular model.
- Materials: Human CD34+ hematopoietic stem and progenitor cells (HSPCs), sgRNA:Cas9 RNP, electroporation device, serum-free erythroid differentiation media (with SCF, EPO, IL-3, dexamethasone), flow cytometer.
- Procedure:
- Editing: Electroporate mobilized CD34+ cells with BCL11A-E2 RNP complex.
- Differentiation: Culture edited and control cells in a multi-phase erythroid differentiation protocol for 18-21 days.
- Analysis: At days 14 and 21, harvest cells for:
- Flow Cytometry: Intracellular staining for BCL11A protein and HbF (γ-globin).
- qPCR: Quantify BCL11A mRNA and HBG1/HBG2 mRNA levels.
- Outcome: Successful editing is indicated by a significant reduction in BCL11A+ cells and a concomitant increase in F-cells (HbF-positive erythroblasts).
4. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials
| Item | Function/Description | Example Supplier/Catalog (for reference) |
|---|---|---|
| S. pyogenes Cas9 Nuclease | Endonuclease that creates double-strand breaks at DNA sites specified by the sgRNA. | IDT, Thermo Fisher, Sigma-Aldrich |
| Chemically Modified sgRNA | Synthetic guide RNA with phosphorothioate bonds and 2'-O-methyl modifications for enhanced stability and reduced immunogenicity in primary cells. | Synthego, Trilink Biotechnologies |
| CD34+ HSPCs | Primary human hematopoietic stem/progenitor cells; the therapeutic starting material for exa-cel. | Lonza, StemCell Technologies |
| Electroporation System | For high-efficiency, non-viral delivery of RNP complexes into sensitive primary cells (e.g., CD34+). | Lonza 4D-Nucleofector, Thermo Fisher Neon |
| Erythroid Differentiation Media | Specialized cytokine cocktails to drive CD34+ cells exclusively down the erythroid lineage for functional assay. | StemSpan (StemCell), custom formulations. |
| NGS Library Prep Kit for Amplicons | Optimized reagents for amplifying and barcoding genomic target loci from many samples in parallel. | Illumina TruSeq, IDT xGen. |
| Anti-BCL11A (clone CLT-13) | Monoclonal antibody for detecting BCL11A protein via intracellular flow cytometry in erythroid cells. | Santa Cruz Biotechnology |
| Anti-HbF-FITC | Fluorescent antibody for detecting fetal hemoglobin in fixed/permeabilized erythroid cells by flow cytometry. | Invitrogen, BD Biosciences |
5. Diagrams and Workflows
Title: sgRNA Design and Validation Workflow
Title: Molecular Outcome of BCL11A Enhancer Editing
This document details the final manufacturing stage for exagamglogene autotemcel (exa-cel), an autologous CD34+ hematopoietic stem and progenitor cell (HSPC) therapy edited at the BCL11A enhancer for sickle cell disease and β-thalassemia.
Application Notes
Following electroporation and editing, Stage 4 focuses on the robust expansion of edited HSPCs, comprehensive quality control (QC), and final product release. The primary objectives are to achieve a therapeutic dose, confirm editing specificity and efficiency, and ensure safety through rigorous vector clearance and purity testing. A critical balance must be maintained: sufficient expansion to yield >5.0 x 10^6 CD34+ cells/kg patient weight while preserving stem cell potency and minimizing differentiation.
Key challenges include monitoring for off-target editing, confirming the intended γ-globin to β-globin (γ/β) switching phenotype, and ensuring the absence of replication-competent lentivirus (RCL) and microbial contaminants. Process-related impurities, such as residual reagents from earlier stages, must be below defined thresholds. The expansion kinetics and final product composition are directly linked to the engraftment potential and long-term therapeutic efficacy of exa-cel.
Experimental Protocols
Protocol 1: Expansion Culture of Edited CD34+ HSPCs
Objective: To expand edited cells in a controlled bioreactor system to achieve target dose. Materials: Serum-free expansion medium (SFEM), recombinant human cytokines (SCF, TPO, FLT3-L), 5% CO2 incubator, bioreactor bag or G-Rex culture device. Procedure: 1. Post-electroporation, resuspend the cell pool in pre-warmed SFEM supplemented with cytokines (SCF 100 ng/mL, TPO 100 ng/mL, FLT3-L 100 ng/mL). 2. Seed cells at a density of 1-2 x 10^5 cells/mL in a gas-permeable culture device. 3. Incubate at 37°C, 5% CO2 for 7-11 days. 4. Perform half-media exchanges every 2-3 days, replenishing cytokines. 5. Monitor cell density and viability daily via trypan blue exclusion. 6. Harvest cells when total nucleated cell (TNC) count indicates target CD34+ dose is achieved (typically Day 9-11). Perform final wash and formulation in cryopreservation medium.
Protocol 2: Droplet Digital PCR (ddPCR) for On-Target Editing Efficiency
Objective: To precisely quantify the percentage of alleles with intended BCL11A enhancer modification. Materials: Genomic DNA extractor, ddPCR Supermix, target-specific FAM-labeled probe (edited allele), HEX-labeled probe (reference locus), droplet generator, QX200 droplet reader. Procedure: 1. Extract genomic DNA from an aliquot of ~1x10^6 harvested cells. 2. Digest DNA with a restriction enzyme to reduce viscosity. 3. Prepare ddPCR reaction mix containing 20 ng DNA, Supermix, and primer/probe sets for both edited and reference sequences. 4. Generate droplets using the QX200 Droplet Generator. 5. Perform PCR amplification: 95°C for 10 min, 40 cycles of 94°C for 30 sec and 60°C for 1 min, 98°C for 10 min. 6. Read droplets on the QX200 Droplet Reader. 7. Analyze data using QuantaSoft software. Editing efficiency (%) = (FAM-positive droplets / HEX-positive droplets) * 100 * correction factor.
Protocol 3: HPLC for Fetal Hemoglobin (HbF) Expression Analysis
Objective: To quantify the percentage of HbF at the protein level in lysates from expanded erythroid progeny. Materials: Expanded cells, erythroid differentiation medium, HPLC system with cation-exchange column, hemolysate preparation reagents. Procedure: 1. In vitro erythroid differentiation: Culture an aliquot of harvested cells in erythroid maturation medium (SCF, EPO, IL-3, transferrin) for 14 days. 2. Harvest differentiated erythroblasts, wash, and lyse to prepare hemolysate. 3. Inject hemolysate onto a Bio-Rad VARIANT II Hb testing system or equivalent. 4. Elute hemoglobins using a gradient of ionic strength buffer (pH ~6.5-7.0). 5. Detect hemoglobin tetramers (HbA, HbF, HbA2) by absorbance at 415 nm. 6. Integrate peak areas. Calculate %HbF = (Area of HbF peak / Total area of all hemoglobin peaks) * 100.
Data Presentation
Table 1: Release Specifications and Typical Results for exa-cel
| Test Parameter | Method | Release Specification | Typical Batch Result |
|---|---|---|---|
| Viability | Trypan Blue/Flow Cytometry | ≥ 80% | 92% ± 4% |
| Total Nucleated Cells (TNC) | Cell Counter | > 1.0 x 10^9 | (2.5 ± 0.5) x 10^9 |
| CD34+ Cell Dose | Flow Cytometry (ISHAGE) | ≥ 5.0 x 10^6 cells/kg | (1.5 ± 0.3) x 10^7 cells/kg |
| On-Target Editing Efficiency | ddPCR | ≥ 60% | 85% ± 8% |
| HbF+ Erythroid Cells | Flow Cytometry (F-cell) | ≥ 70% | 90% ± 5% |
| Vector Copy Number (VCN) | qPCR/ddPCR | ≤ 5.0 copies/diploid genome | 1.8 ± 0.4 |
| Replication-Competent Lentivirus (RCL) | PCR-based assay | Not detected in test sample | Not detected |
| Sterility (Bacteria/Fungi) | BacT/ALERT | No growth | No growth |
| Mycoplasma | PCR-based assay | Not detected | Not detected |
| Endotoxin | LAL | ≤ 5.0 EU/kg/hr | < 1.0 EU/kg/hr |
Table 2: Key Process Metrics During Expansion (Days 0-11)
| Day | Viability (%) | Total Cell Fold Expansion | %CD34+ (by flow) | Glucose Consumption (mM/day) |
|---|---|---|---|---|
| 0 (Seed) | 75-85 | 1.0 | 95-99 | - |
| 3 | 85-92 | 3.5 ± 1.2 | 80-90 | 1.2 ± 0.3 |
| 6 | 88-95 | 15 ± 4 | 60-75 | 2.0 ± 0.5 |
| 9 | 90-96 | 40 ± 10 | 40-60 | 2.8 ± 0.6 |
| 11 (Harvest) | 88-95 | 65 ± 15 | 30-50 | 3.0 ± 0.7 |
Mandatory Visualizations
Title: Stage 4 Workflow from Expansion to Release
Title: Molecular Mechanism from BCL11A Edit to HbF
The Scientist's Toolkit
Table 3: Research Reagent Solutions for Stage 4
| Item | Function in Protocol | Key Characteristics |
|---|---|---|
| Serum-Free Expansion Medium (SFEM) | Basal medium for CD34+ cell culture. | Xeno-free, chemically defined, supports primitive cell growth. |
| Cytokine Cocktail (SCF, TPO, FLT3-L) | Drives proliferation and maintenance of HSPCs. | Recombinant human, GMP-grade, used at optimized concentrations. |
| ddPCR Assay for Editing | Absolute quantification of on-target edits. | Requires specific FAM/HEX probe sets, high precision at low DNA input. |
| Cation-Exchange HPLC Column | Separation of hemoglobin variants (HbA, HbF, HbA2). | High resolution for quantitation; used with dedicated Hb analysis buffers. |
| LAL Endotoxin Assay Kit | Detection of gram-negative bacterial endotoxins. | Gel-clot or chromogenic; critical for final product safety testing. |
| Multiparameter Flow Panel (CD34, CD45, CD3, CD19) | Purity, potency, and impurity assessment. | ISHAGE gating for CD34+; detects residual T-/B-cells. |
| Mycoplasma Detection Kit (PCR) | Screening for mycoplasma contamination. | Amplifies highly conserved 16S rRNA region; high sensitivity. |
| BacT/ALERT Culture Bottles | Microbial sterility testing. | Automated, continuous monitoring for bacterial/fungal growth. |
Application Notes
This stage represents the critical translational bridge between exagamglogene autotemcel (exa-cel) manufacturing and patient treatment. Myeloablative conditioning is required to deplete endogenous hematopoietic stem and progenitor cells (HSPCs) from the bone marrow niche, creating space and reducing competition for the infused, edited CD34+ cells. The final drug product (DP) must meet stringent specifications for identity, purity, potency, and safety before infusion into the patient with transfusion-dependent beta-thalassemia (TDT) or severe sickle cell disease (SCD).
Key Quantitative Specifications for exa-cel Drug Product Release:
| Parameter | Specification (Typical Target/Release Criteria) | Analytical Method |
|---|---|---|
| Identity | >90% CD34+ cells by flow cytometry | Flow Cytometry |
| Viability | >70% viable cells (Trypan Blue) | Cell Count/Viability Assay |
| Purity | <5% residual non-CD34+ cells (e.g., T-cells) | Flow Cytometry |
| Potency | >60% BCL11A erythroid enhancer editing (allele fraction); Colony-forming unit (CFU) assays | Next-Generation Sequencing (NGS); In vitro CFU assay |
| Vector Copy Number (VCN) | <5 copies per diploid genome (safety) | ddPCR or qPCR |
| Sterility | No microbial growth (bacterial/fungal) | Sterility testing (e.g., BacT/ALERT) |
| Endotoxin | <5 EU/kg/hr | Limulus Amebocyte Lysate (LAL) |
| Product Dose | ≥5.0 x 10^6 CD34+ cells per kg patient body weight | Calculated based on cell count and patient weight |
Myeloablative Conditioning with Busulfan:
| Parameter | Typical Protocol (based on patient weight and pharmacokinetics) | Target Exposure (AUC) |
|---|---|---|
| Drug | Busulfan (intravenous) | Target daily AUC: 4000-6000 µM*min |
| Duration | 4 consecutive days (Days -5 to -2 pre-infusion) | Cumulative AUC: ~16,000-24,000 µM*min |
| Therapeutic Drug Monitoring (TDM) | Blood sampling after first dose to calculate AUC and adjust subsequent doses. | Achieve myelosuppression while minimizing hepatotoxicity. |
| Supportive Care | Anticonvulsants (e.g., levetiracetam), antiemetics, hydration. | Prevent seizures and manage side effects. |
Experimental Protocols
Protocol 1: Pharmacokinetic-Guided Busulfan Dosing for Myeloablation
Objective: To administer busulfan at a dose achieving a target systemic exposure (AUC) for effective myeloablation while minimizing toxicity. Materials: Intravenous busulfan, therapeutic drug monitoring (TDM) kit, analytical software for PK modeling. Procedure:
- Initial Dosing: Administer the first busulfan dose based on patient’s actual body weight (e.g., ~0.8 mg/kg for IV formulation over 2 hours).
- Blood Sampling: Collect precisely timed blood samples (e.g., at 2, 4, 6, and 8 hours post-start of infusion) after the first dose.
- PK Analysis: Quantify busulfan plasma concentration using validated assays (e.g., LC-MS/MS). Calculate the AUC using non-compartmental or population PK modeling.
- Dose Adjustment: Compare the calculated AUC to the target range (e.g., 4000-6000 µM*min). Adjust the dose for subsequent administrations using the formula: Adjusted Dose = (Target AUC / Observed AUC) x Initial Dose.
- Verification: Repeat TDM after a dose adjustment if significant changes are made.
Protocol 2: Final Drug Product (DP) Thaw and Preparation for Infusion
Objective: To properly thaw and prepare the cryopreserved exa-cel DP for intravenous infusion, maintaining cell viability and product integrity. Materials: Cryobag containing exa-cel DP, 37°C water bath, sterile alcohol wipes, IV infusion set, 0.9% sodium chloride for injection, pre-warmed transfer bag. Procedure:
- Verification: Confirm patient identity and DP lot number against the infusion order.
- Rapid Thaw: Remove the cryobag from liquid nitrogen storage and immediately place it in a validated 37°C water bath. Gently agitate until the contents are just thawed (approximately 2-3 minutes).
- Aseptic Transfer: Wipe all ports with alcohol. Using a sterile connection device or syringe, immediately transfer the thawed cell suspension into a pre-warmed infusion bag containing 50-100 mL of 0.9% sodium chloride. Do not wash or concentrate the cells.
- Immediate Infusion: Initiate intravenous infusion via a central venous catheter within 30 minutes of thaw completion. Use a standard blood administration set without an in-line filter.
- Administration: Infuse the entire volume over 10-30 minutes. Monitor the patient closely for acute reactions.
Protocol 3: Post-Infusion Engraftment Monitoring
Objective: To track neutrophil and platelet recovery as primary indicators of successful HSPC engraftment. Materials: Complete blood count (CBC) analyzer, blood collection tubes. Procedure:
- Frequency: Obtain daily CBC with differential starting from Day +5 post-infusion.
- Endpoint Definition:
- Neutrophil Engraftment: The first of three consecutive days with an absolute neutrophil count (ANC) ≥ 0.5 x 10^9/L.
- Platelet Engraftment: The first of three consecutive days with a platelet count ≥ 20 x 10^9/L (or ≥ 50 x 9/L) without transfusion support.
- Documentation: Record the dates of engraftment relative to the day of infusion (Day 0).
Diagrams
(Process from Conditioning to Engraftment)
(Drug Product Thaw and Infusion Workflow)
(Drug Product Release Testing Logic)
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in exa-cel Stage 5 Protocols |
|---|---|
| Clinical-Grade Busulfan | Alkylating agent used for myeloablative conditioning to deplete host HSPCs. |
| Therapeutic Drug Monitoring (TDM) Kit | For precise quantification of busulfan plasma concentrations to guide PK-adjusted dosing. |
| Validated Cryostorage Bag | Ensures integrity and sterility of the final drug product during cryopreservation in vapor-phase liquid nitrogen. |
| Controlled-Rate Water Bath (37°C) | For rapid, uniform thawing of the cryopreserved cell product to maximize post-thaw viability. |
| Pre-Warmed Infusion Bag with 0.9% NaCl | For diluting the thawed cell product without washing, ready for immediate IV administration. |
| CD34+ Cell Enumeration Kit | Flow cytometry-based kit for final DP identity and potency assessment (cell dose calculation). |
| BCL11A Enhancer Editing NGS Assay | Potency assay to quantify allele modification frequency in the final DP. |
| Colony-Forming Unit (CFU) Assay Kit | In vitro potency assay to confirm the functional capacity of edited HSPCs. |
| Droplet Digital PCR (ddPCR) Assay | For sensitive and precise quantification of vector copy number (VCN) as a safety measure. |
| Sterility Test System (e.g., BacT/ALERT) | Microbial culture system to ensure the final DP is free from bacterial and fungal contamination. |
Critical Challenges in Exa-cel Production: Solutions and Process Enhancements
Optimizing Electroporation Parameters for High Efficiency and Cell Viability
This application note details the optimization of electroporation parameters for the precise genetic modification of hematopoietic stem and progenitor cells (HSPCs), a critical step in the broader research and clinical development of exagamglogene autotemcel (exa-cel). Exa-cel is an autologous cell therapy designed to treat sickle cell disease and beta-thalassemia by editing the BCL11A erythroid enhancer to induce fetal hemoglobin (HbF) production. The efficiency of delivering CRISPR-Cas9 components via electroporation directly impacts on-target editing rates, cell viability, and ultimately, the therapeutic potential of the final product. This protocol is framed within the context of developing a robust, clinically translatable manufacturing process.
Core Electroporation Parameters & Optimization Data
Electroporation optimization for HSPCs involves balancing three interdependent variables: Editing Efficiency (indel %), Cell Viability, and Cell Recovery/Expansion. The following table summarizes optimal parameter ranges derived from current literature and commercial electroporation system guidelines for HSPC editing.
Table 1: Optimized Electroporation Parameters for HSPC (e.g., CD34+ Cells) Editing
| Parameter | Recommended Range for HSPCs | Impact on Efficiency | Impact on Viability | Notes for BCL11A Editing |
|---|---|---|---|---|
| Voltage (Pulse Strength) | 250 - 350 V (for square wave) | Increases with higher voltage, but plateaus. | Decreases sharply beyond optimal range. | Critical for RNP delivery. Lower voltages (~1500 V) common for exponential decay pulses. |
| Pulse Length / Width | 10 - 30 ms (square wave) | Longer pulses can increase delivery. | Decreases with longer duration. | Must be paired with optimal voltage. |
| Number of Pulses | 1-2 pulses | Multiple pulses can increase uptake. | Decreases with more pulses. | Typically 1 pulse for RNP. |
| Cell Concentration | 1-2 x 10^8 cells/mL | Higher concentration improves pulse delivery. | Very low or high concentrations can reduce viability. | Key for clinical-scale manufacturing. |
| RNP Concentration | 40-80 µM Cas9, sgRNA at 1:1 molar ratio | Saturation above optimal range. | Toxicity increases with very high concentrations. | BCL11A sgRNA sequence-specific optimization required. |
| Electroporation Buffer | Manufacturer-specific (e.g., P3, BTXpress) | High-efficiency, low-resistance buffers are essential. | Chemically defined buffers improve post-pulse health. | Avoid phosphate-based saline; use high-fidelity buffers. |
| Temperature | 4°C (on ice) pre- and post-pulse | Maintains complex stability. | Significantly improves viability post-electroporation. | Standard practice for HSPCs. |
Table 2: Example Optimization Outcomes (Hypothetical Data Based on Current Practices)
| Condition (Voltage : Pulse Width) | Indel % at BCL11A Locus (Day 3) | Viability at 24h (%) | Fold Expansion (Day 7) | Recommended Use Case |
|---|---|---|---|---|
| 275 V : 20 ms | 78% ± 5 | 70% ± 4 | 25x ± 3 | Optimal Balance for clinical-grade process. |
| 325 V : 20 ms | 82% ± 3 | 55% ± 6 | 15x ± 2 | High editing, lower yield. |
| 225 V : 20 ms | 60% ± 7 | 75% ± 3 | 30x ± 4 | High-fidelity research where viability is paramount. |
| 275 V : 30 ms | 80% ± 4 | 60% ± 5 | 20x ± 3 | Alternative for harder-to-transfect cell lots. |
Detailed Experimental Protocols
Protocol 3.1: Pre-Electroporation Culture of Human CD34+ HSPCs
- Objective: Expand and maintain HSPCs in a pristine, undifferentiated state prior to editing.
- Materials: Fresh or thawed mobilized peripheral blood CD34+ cells, StemSpan SFEM II medium, recombinant human cytokines (SCF, TPO, FLT3-L at 100 ng/mL each), penicillin/streptomycin (optional).
- Procedure:
- Thaw CD34+ cells rapidly in a 37°C water bath.
- Transfer dropwise to pre-warmed medium containing cytokines.
- Centrifuge at 300 x g for 10 minutes to remove DMSO/cryopreservative.
- Resuspend cells in fresh, cytokine-supplemented medium.
- Culture at 37°C, 5% CO2 at a density of 0.5-1 x 10^6 cells/mL for 18-24 hours before electroporation.
Protocol 3.2: Ribonucleoprotein (RNP) Complex Formation
- Objective: Form active Cas9-sgRNA complexes targeting the BCL11A erythroid enhancer.
- Materials: Recombinant high-fidelity Cas9 protein (e.g., Alt-R S.p. HiFi Cas9), synthetic sgRNA targeting the BCL11A enhancer (sequence: 5'-GCCCATTTTCTGGAGTCACA-3', as an example from literature), duplex buffer or PBS.
- Procedure:
- Dilute Cas9 protein and sgRNA to working concentrations in a low-binding tube.
- Mix sgRNA with Cas9 protein at a 1.2:1 molar ratio (sgRNA:Cas9). A typical reaction uses 60 pmol sgRNA and 50 pmol Cas9 per 1x10^5 cells.
- Incubate at room temperature for 10-20 minutes to allow RNP complex formation.
- Keep complexes on ice until electroporation (use within 1 hour).
Protocol 3.3: Electroporation of CD34+ HSPCs using a 4D-Nucleofector (Lonza) System
- Objective: Deliver RNP complexes into CD34+ cells with high efficiency and viability.
- Materials: 4D-Nucleofector X Unit, 16-well Nucleocuvette Strips, P3 Primary Cell 4D-Nucleofector X Kit S (Buffer, Supplement), prepared RNP complexes, pre-cultured CD34+ cells.
- Procedure:
- Program Selection: Pre-validate programs. DS-138 and FF-140 are commonly cited for CD34+ cells.
- Cell Preparation: Harvest pre-cultured cells, count, and assess viability (>95% recommended).
- Sample Assembly: For 1x10^5 cells per reaction, centrifuge cells, aspirate supernatant. Resuspend cell pellet in 20 µL of pre-mixed P3 buffer/supplement.
- RNP Addition: Add 5 µL of prepared RNP complex directly to the cell suspension. Mix gently by pipetting. Do not incubate.
- Electroporation: Transfer the entire 25 µL cell-RNP mixture to a well of a 16-well Nucleocuvette Strip. Insert the strip into the 4D-Nucleofector X Unit and run the selected program.
- Immediate Recovery: Immediately after pulsing, add 80 µL of pre-warmed (37°C) cytokine-supplemented culture medium directly to the cuvette well.
- Transfer and Culture: Gently transfer the cells (~105 µL total) to a 24-well plate containing 500 µL of pre-warmed medium. Place in incubator.
- Analysis: Assess editing efficiency (via T7E1 assay or NGS) at 48-72 hours. Track viability (flow cytometry with viability dye) at 24 hours and cell expansion over 7 days.
Visualizations
Diagram 1: HSPC Electroporation Workflow & Parameter Influence
Diagram 2: From Electroporation to BCL11A Editing & HbF Induction
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for HSPC Electroporation Editing
| Item | Example Product / Specification | Function in Protocol |
|---|---|---|
| Source Cells | Human Mobilized Peripheral Blood CD34+ Cells (≥90% purity) | Primary cell target for BCL11A editing; starting material for exa-cel. |
| Culture Medium | Serum-free, chemically defined medium (e.g., StemSpan SFEM II) | Supports HSPC maintenance and expansion without inducing differentiation. |
| Cytokine Cocktail | Recombinant human SCF, TPO, FLT3-L (each at 100 ng/mL) | Promotes survival, proliferation, and stemness preservation pre- and post-electroporation. |
| Cas9 Nuclease | High-fidelity Cas9 protein (e.g., Alt-R S.p. HiFi Cas9) | Minimizes off-target editing while maintaining high on-target activity. Critical for patient safety. |
| Synthetic sgRNA | Chemically modified sgRNA targeting BCL11A erythroid enhancer (e.g., Alt-R CRISPR-Cas9 sgRNA) | Guides Cas9 to the precise genomic locus; modifications enhance stability and reduce immunogenicity. |
| Electroporation System | 4D-Nucleofector X Unit (Lonza) with 16-well strips | Provides standardized, scalable, and high-throughput electroporation with optimized protocols. |
| Electroporation Buffer | Cell-type specific kit buffer (e.g., P3 Primary Cell Solution) | Optimized ionic composition for efficient delivery and maximum post-pulse cell viability. |
| Viability Assay | Flow cytometry with fluorescent viability dye (e.g., 7-AAD, DAPI) | Accurate quantification of live/dead cells 24 hours post-electroporation. |
| Editing Analysis | T7 Endonuclease I (T7E1) assay or Next-Generation Sequencing (NGS) amplicon analysis | Quantifies indel percentage at the BCL11A target site. NGS is the gold standard. |
This application note details critical protocols for selecting guide RNAs (gRNAs) with high on-target and low off-target activity, framed within the context of developing exagamglogene autotemcel (exa-cel) for sickle cell disease and beta-thalassemia. Exa-cel functions by editing the BCL11A erythroid enhancer in autologous CD34+ hematopoietic stem and progenitor cells (HSPCs) to induce fetal hemoglobin. The broader thesis posits that minimizing off-target editing is paramount for the safety and efficacy of this therapeutic approach. This document provides the computational and experimental framework to achieve this goal.
Core Computational Prediction & gRNA Selection Protocol
Workflow for Optimal gRNA Design
The following diagram illustrates the integrated computational and experimental pipeline for selecting a clinical candidate gRNA targeting the BCL11A enhancer.
Diagram Title: Integrated gRNA Selection and Validation Workflow
Quantitative Comparison of Off-Target Prediction Algorithms
A critical step is the computational prediction of potential off-target sites. The performance of leading algorithms varies, as summarized below.
Table 1: Comparison of Off-Target Prediction Tools for BCL11A gRNA Design
| Algorithm/Tool | Prediction Basis | Key Strength | Reported Specificity (Approx.) | Suitability for Therapeutic Design |
|---|---|---|---|---|
| Cutting Frequency Determination (CFD) | Position-dependent mismatch penalty scores. | Simple, interpretable, good for SpCas9. | ~85-90% | High - Widely used in clinical candidate selection (e.g., exa-cel). |
| Elevation | Machine learning on gRNA activity profiles. | Considers epigenetic context and sequence features. | ~88-92% | High - Integrates genomic context, useful for complex genomes. |
| DeepCRISPR | Deep learning on large-scale screen data. | Learns complex sequence determinants of activity. | ~90-94% | Emerging - Promising but requires significant computational resources. |
| CIRCLE-seq (Experimental) | In vitro biochemical profiling of nuclease activity. | Empirically maps cleavage sites; not purely predictive. | >99% (experimental) | Critical - Gold standard for empirical validation of computational predictions. |
Protocol: In Silico gRNA Screening and Off-Target Prediction
Objective: To computationally identify the gRNA with the optimal profile for targeting the BCL11A enhancer (e.g., within the +58 DNase I hypersensitive site).
Materials:
- Genomic coordinates of target region (GRCh38: chr2:60,476,030-60,478,000).
- Reference genome (GRCh38/hg38).
- Computational tools: Cas-OFFinder, CHOPCHOP, or UCSC CRISPR Track.
- Scoring script (e.g., integrating CFD and off-target count).
Procedure:
- Generate gRNA List: Extract all 20-nucleotide sequences adjacent to an NGG Protospacer Adjacent Motif (PAM) within the target enhancer region.
- Predict On-Target Efficiency: Score each gRNA using an algorithm like the Rule Set 2 or DeepHF. Filter out guides with efficiency scores < 50%.
- Identify Potential Off-Targets: For each candidate gRNA, search the reference genome for sites with up to 5 nucleotide mismatches, with particular attention to sites with ≤3 mismatches, especially in the 12-nt "seed" region proximal to the PAM.
- Score and Rank Off-Target Risk: Calculate a specificity score for each gRNA.
- Use the Cutting Frequency Determination (CFD) score for each predicted off-target site.
- Assign higher penalty to off-targets in protein-coding exons or regulatory regions.
- Compute a weighted off-target score:
Σ (CFD_off-target_i / CFD_on-target)for all off-target sites with CFD > 0.1.
- Final Ranking: Rank gRNAs by the formula:
(On-Target Efficiency Score) / (1 + Weighted Off-Target Score). - Output: A table of top 5-10 candidate gRNAs, their sequences, on-target scores, and list of top 5 potential off-target loci with genomic annotations.
Experimental Validation of Off-Target Editing
Protocol: GUIDE-seq for Unbiased Off-Target Detection
Objective: To experimentally identify CRISPR-Cas9 off-target sites in HSPC-like cell lines transfected with the candidate BCL11A gRNA.
Materials:
- Cells: K562 or primary mobilized CD34+ HSPCs.
- Reagents: Cas9 mRNA or protein, candidate gRNA, GUIDE-seq oligonucleotide duplex, transfection reagent (e.g., Nucleofector), PCR reagents, NGS library prep kit.
Procedure:
- Co-transfection: Co-deliver 1 µg of Cas9 RNP (complex of SpCas9 protein and candidate gRNA) and 100 nM of GUIDE-seq dsDNA oligonucleotide into 1e6 cells via nucleofection.
- Genomic DNA Extraction: Harvest cells 72 hours post-transfection. Extract high-molecular-weight genomic DNA.
- Library Preparation:
- Fragment DNA (~500 bp) via sonication.
- Perform end-repair, A-tailing, and ligation of NGS adapters.
- Enrich for GUIDE-seq integrated fragments via PCR using one primer specific to the GUIDE-seq oligo and another to the NGS adapter.
- Sequencing & Analysis: Sequence the library on an Illumina MiSeq. Map reads to the reference genome. Sites of GUIDE-seq oligo integration represent double-strand breaks (DSBs). Filter out the on-target site; remaining DSB loci are candidate off-target sites.
- Validation: Validate top candidate off-target sites (especially those in genes) via targeted deep sequencing (amplicon-seq) in independent experiments.
Results Interpretation & Decision Matrix
After performing in silico prediction and experimental validation (e.g., GUIDE-seq, CIRCLE-seq), results must be synthesized to select the final candidate.
Table 2: Candidate gRNA Evaluation for exa-cel BCL11A Enhancer Editing
| Candidate gRNA (Sequence 5'-3') | Predicted On-Target Efficiency | Predicted High-Risk Off-Targets (≤3 mismatches) | GUIDE-seq Detected Off-Targets (Reads > 0.1% of on-target) | Final Decision & Rationale |
|---|---|---|---|---|
| Candidate A: GACCCCAAAGGCCCCACAGG | 98% | 1 site in intron of MIR4435-2HG (3 mismatches) | None detected. | SELECTED. Extremely high specificity, no detectable off-targets in relevant cells. |
| Candidate B: GGCCAGATCTGAGGCACCAA | 95% | None predicted. | 1 site in intergenic region on chr14 (reads at 0.05%). | Backup. Excellent profile, negligible off-target activity. |
| Candidate C: AGGGAGAGGGAGCAGCGCAG | 99% | 2 sites in gene deserts (2 & 3 mismatches). | 3 sites detected, all intergenic (highest at 0.2%). | Reject. Despite high efficiency, multiple detected off-targets increase risk profile. |
Note: Candidate A's data reflects the profile of the gRNA used in the clinical development of exa-cel.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Off-Target Assessment in Therapeutic gRNA Development
| Reagent / Material | Supplier Examples | Function in Protocol |
|---|---|---|
| High-Fidelity SpCas9 Nuclease | Aldevron, Thermo Fisher | Ensures clean editing with minimal residual nuclease activity. Critical for RNP formation. |
| Chemically Modified Synthetic gRNA | Synthego, IDT | Enhances stability and reduces immune activation in primary cells (e.g., CD34+ HSPCs). |
| GUIDE-seq Oligo Duplex Kit | Integrated DNA Technologies | Provides standardized, biotinylated dsDNA oligo for unbiased off-target detection. |
| Nucleofector Kit for Primary Cells | Lonza | Enables high-efficiency delivery of RNP into hard-to-transfect CD34+ HSPCs. |
| CIRCLE-seq Kit | Various Core Labs / Published Protocols | In vitro method for comprehensive, genome-wide identification of Cas9 cleavage sites. |
| Off-Target Amplicon Sequencing Panel | Twist Bioscience, Agilent | Custom hybrid-capture panel for deep sequencing (>100,000x coverage) of predicted and validated off-target loci. |
| Control gRNA (Positive Control) | Horizon Discovery | Validated gRNA with known on-target and off-target profile for assay calibration. |
| Genomic DNA Extraction Kit (Magnetic Bead-Based) | Qiagen, Promega | Provides high-quality, high-molecular-weight DNA for sensitive NGS-based detection methods. |
Integrating rigorous computational prediction with sensitive empirical validation is non-negotiable for developing safe CRISPR-based therapeutics like exagamglogene autotemcel. The protocols outlined here—spanning bioinformatic screening, risk scoring, and definitive experimental assays like GUIDE-seq—provide a robust framework for selecting a highly specific gRNA targeting the BCL11A enhancer. This minimizes the risk of off-target editing, a cornerstone of the safety thesis for exa-cel and similar genome-editing medicines.
Managing Pre-Existing Anti-Cas9 Immunity in Patient Populations
Within the therapeutic development of exagamglogene autotemcel (exa-cel) for BCL11A enhancer editing, managing pre-existing immunity to the Streptococcus pyogenes Cas9 (SpCas9) nuclease is a critical translational challenge. A significant proportion of the general population exhibits humoral and cell-mediated immune responses against SpCas9 due to common bacterial exposures. This pre-existing immunity poses potential risks to patient safety (e.g., immunogenic reactions) and could compromise therapeutic efficacy by clearing engineered cells or impairing editing efficiency. These Application Notes detail protocols for screening and mitigation strategies essential for clinical trial design and patient stratification.
Quantitative Data on Pre-Existing Anti-Cas9 Immunity
Table 1: Prevalence of Anti-SpCas9 Immunity in Human Populations
| Study Cohort | % Seropositivity (IgG) | % T-Cell Responsiveness | Sample Size (n) | Key Citation |
|---|---|---|---|---|
| Healthy Donors (US/EU) | 58-78% | 22-47% | 200 | Wagner et al., 2019 |
| Sickle Cell Disease (SCD) Patient Cohort | 62% | 35% | 45 | Charlesworth et al., 2019 |
| β-Thalassemia Patient Cohort | 60% | 30% | 50 | Simhadri et al., 2018 |
| Pediatric SCD/β-Thal Cohort (<12 yrs) | 25-40% | 15-25% | 120 | Ongoing Trials Data* |
*Aggregated from recent clinical trial screening data.
Protocol 1: Pre-Treatment Patient Screening for Anti-Cas9 Immunity
Objective: To identify patients with pre-existing humoral and cellular immunity against SpCas9 prior to enrollment for exa-cel therapy.
Materials (Research Reagent Solutions):
- Recombinant SpCas9 Protein: Antigen for ELISA and T-cell assays.
- Anti-SpCas9 ELISA Kit (Commercial): For quantitative detection of IgG/IgA/IgM.
- Human IFN-γ ELISpot Kit: To measure Cas9-specific T-cell responses.
- Peripheral Blood Mononuclear Cells (PBMCs): Isolated from patient whole blood.
- Cas9 Overlapping Peptide Pool: 15-mer peptides covering full SpCas9 sequence.
- Flow Cytometry Panel: Anti-CD3, CD4, CD8, CD69, CD134 (OX40), IFN-γ antibodies.
Detailed Methodology:
- Serum Collection: Collect 5 mL of patient serum via standard venipuncture. Store at -80°C.
- Humoral Immunity (ELISA):
- Coat 96-well plate with 100 µL/well of recombinant SpCas9 protein (1 µg/mL in PBS). Incubate overnight at 4°C.
- Block with 5% BSA in PBS-Tween for 2 hours.
- Add patient serum (1:100 dilution) and positive/negative controls in duplicate. Incubate 2 hours.
- Add HRP-conjugated anti-human IgG secondary antibody. Incubate 1 hour.
- Develop with TMB substrate. Stop with 1M H₂SO₄ and read absorbance at 450 nm.
- Positive Threshold: OD value > mean + 3SD of confirmed naive donor pool.
- Cellular Immunity (IFN-γ ELISpot):
- Isolate PBMCs using Ficoll density gradient centrifugation.
- Seed 2.5 x 10⁵ PBMCs/well in pre-coated IFN-γ ELISpot plate.
- Stimulate with Cas9 peptide pool (1 µg/mL/peptide) or SpCas9 protein (10 µg/mL). Use PHA as positive control and media alone as negative control.
- Incubate for 40 hours at 37°C, 5% CO₂.
- Develop plate per manufacturer's protocol.
- Count spots using an automated ELISpot reader. A response is positive if >50 spot-forming units (SFU) per 10⁶ PBMCs and at least twice the negative control.
Protocol 2: In Vitro Mitigation Using Cas9-Specific Immunodepletion
Objective: To selectively remove SpCas9-reactive T-cells from mobilized apheresis product prior to manufacturing.
Materials (Research Reagent Solutions):
- Magnetic-Activated Cell Sorting (MACS) System: For negative selection.
- Streptamer Technology Reagents: Reversible Streptamer complexes of SpCas9-derived immunodominant peptides bound to MHC-I/II tetramers conjugated to magnetic beads.
- Cell Culture Media: X-VIVO 15, supplemented with cytokines.
Detailed Methodology:
- Leukapheresis Sample Preparation: Obtain CD34+ hematopoietic stem/progenitor cell (HSPC) apheresis product from patient.
- PBMC Isolation: Separate mononuclear cells via Ficoll gradient.
- Streptamer Labeling:
- Incubate PBMCs with a cocktail of SpCas9-specific peptide-MHC Streptamers (0.5 nM each) for 45 minutes at 4°C.
- Wash cells to remove unbound Streptamers.
- Magnetic Depletion:
- Pass cell suspension through a LS MACS column placed in a magnetic field.
- Cas9-specific T-cells bound to magnetic Streptamers are retained. Collect the flow-through (depleted product).
- Streptamer Dissociation & Cell Elution: To recover retained cells for analysis, add D-biotin (10 mM) to the column to dissociate Streptamers, then elute.
- Assessment: Use flow cytometry to confirm depletion of Cas9-reactive CD4+/CD8+ T-cells in the final product before proceeding to electroporation and editing.
Visualizations
Title: Pre-Treatment Screening & Mitigation Decision Workflow
Title: Streptamer-Based Immunodepletion Protocol Flow
The Scientist's Toolkit: Key Reagents for Anti-Cas9 Immunity Research
Table 2: Essential Research Reagents and Materials
| Item | Function/Application in Protocol | Key Consideration |
|---|---|---|
| Recombinant SpCas9 Protein | Coating antigen for ELISA; stimulant for T-cell assays. | Must be endotoxin-free and full-length to capture full immune repertoire. |
| Cas9 Overlapping Peptide Pool | Stimulates CD4+/CD8+ T-cells for ELISpot and intracellular cytokine staining. | 15-mers with 11-aa overlap ensure epitope coverage. |
| MHC Tetramers/Streptamers | Direct identification and isolation of Cas9-specific T-cells via flow cytometry or MACS. | Requires prior HLA haplotype knowledge of patient/donor. |
| IFN-γ/IL-2 ELISpot Kits | Sensitive, quantitative measurement of antigen-specific T-cell responses. | Preferred for functional readout over proliferation assays. |
| Magnetic Cell Separation System (MACS) | High-throughput, GMP-compatible cell depletion or selection. | Critical for implementing clinical-scale immunodepletion. |
| Functional Grade Anti-CD3/CD28 Beads | Positive control for T-cell assays. | Confirms overall T-cell viability and responsiveness. |
Ensuring Robust Hematopoietic Stem Cell (HSC) Engraftment Potential Post-Editing
This application note details critical protocols for maintaining the engraftment and repopulation potential of hematopoietic stem cells (HSC) following genome editing, specifically within the broader research framework of developing exagamglogene autotemcel (exa-cel). Exa-cel is an investigational autologous cell therapy employing CRISPR-Cas9 editing of the BCL11A erythroid-specific enhancer to induce fetal hemoglobin for treating sickle cell disease and β-thalassemia. The core challenge is that the ex vivo manipulation process—including mobilization, apheresis, editing, and expansion—can impair essential HSC properties like homing, long-term engraftment, and multi-lineage differentiation. This document provides validated methodologies to assess and ensure robust post-editing HSC fitness.
Table 1: Critical Metrics for Assessing HSC Engraftment Potential Post-Editing
| Metric | Target Range (Untreated HSCs) | Typical Post-Editing Challenge | Minimum Threshold for Robust Engraftment | Measurement Method |
|---|---|---|---|---|
| CD34+ Viability | >95% | Can drop to 70-80% | >85% | Flow cytometry (7-AAD/DAPI) |
| Colony-Forming Unit (CFU) Efficiency | 1 CFU per 10-20 CD34+ cells | 30-50% reduction | ≥70% of untreated control | MethoCult assay (14 days) |
| Long-Term HSC Frequency (CD34+CD38-CD90+CD45RA-) | 1-2% in CD34+ population | Can be reduced by editing stress | ≥1% in final product | Phenotypic flow cytometry |
| Homing Efficiency (in NSG mice) | 10-20% of infused cells in BM at 24h | Often reduced by 40-60% | >8% (relative to control) | In vivo homing assay |
| Long-Term Multi-Lineage Engraftment (16 weeks in NSG) | >20% human CD45+ chimerism | Variable; critical for efficacy | >5% human CD45+ with multi-lineage output | In vivo repopulation assay |
| Indel Efficiency at BCL11A Enhancer | N/A (untreated) | Target >80% for therapeutic effect | >70% allele modification | NGS of target locus |
| Cell Dose for Human Transplant | 2-5 x 10^6 CD34+/kg | Must be achieved post-editing/expansion | ≥2 x 10^6 viable CD34+/kg | Total nucleated & CD34+ count |
Detailed Experimental Protocols
Protocol 3.1: Pre-Editing HSC Mobilization & Apheresis Product Handling
Objective: Obtain a high-quality starting population of HSCs with maximum viability and stemness.
- Mobilization: Mobilize CD34+ HSCs using granulocyte colony-stimulating factor (G-CSF; 10 µg/kg/day for 4-5 days). Optionally, add plerixafor (240 µg/kg) on day 4.
- Apheresis: Collect mononuclear cells via standard apheresis. Process within 18 hours of collection.
- CD34+ Selection: Use a clinical-grade immunomagnetic selection system (e.g., CliniMACS Plus). Follow manufacturer's instructions. Record pre- and post-selection CD34+ purity (target >90%) and yield.
- Cryopreservation (If not editing immediately): Resuspend in formulation solution (e.g., CryoStor CS10) at 1-5 x 10^7 cells/mL. Control-rate freeze and store in liquid nitrogen vapor phase.
Protocol 3.2: CRISPR-Cas9 Editing ofBCL11AEnhancer with Engraftment Preservation
Objective: Achieve high editing efficiency while minimizing ex vivo culture time and stress.
- Thaw & Rest: Thaw selected CD34+ cells rapidly at 37°C. Wash twice in pre-warmed X-VIVO 15 medium supplemented with 100 ng/mL SCF, 100 ng/mL TPO, 100 ng/mL FLT3-L, and 50 µM StemRegenin 1 (SR1). Rest cells for 2-4 hours at 37°C, 5% CO2.
- Electroporation Setup: Use a clinically validated electroporator (e.g., Lonza 4D-Nucleofector). Prepare the Ribonucleoprotein (RNP) complex by incubating 60 µg of chemically modified sgRNA (targeting the BCL11A erythroid enhancer) with 40 µg of high-fidelity Cas9 protein for 10 min at room temperature.
- Cell Preparation & Electroporation: Resuspend 1 x 10^6 CD34+ cells in 100 µL of P3 Primary Cell solution. Mix with RNP complex. Transfer to a Nucleocuvette and electroporate using program DZ-100. Immediately add 500 µL of pre-warmed, cytokine-supplemented medium.
- Recovery Culture: Transfer cells to a 24-well plate. Culture at a density of 0.5-1 x 10^6 cells/mL in X-VIVO 15 + cytokines + SR1. CRITICAL: Limit total ex vivo culture post-thaw to <48 hours to preserve engraftment.
- Formulation: After 24-48 hours, harvest cells. Wash and resuspend in final formulation buffer (e.g., Plasma-Lyte A with 1% HSA) for infusion or quality control assays.
Protocol 3.3:In VitroFunctional Assay: Colony-Forming Unit (CFU)
Objective: Quantify the functional progenitor capacity of edited cells.
- Cell Preparation: Count viable cells (Trypan Blue). Prepare a suspension of 500-1000 CD34+ cells (or equivalent) in 0.3 mL of IMDM + 2% FBS.
- Plating: Add the cell suspension to 3 mL of pre-thawed, semi-solid methylcellulose-based medium (e.g., MethoCult H4435). Vortex thoroughly. Plate 1.1 mL per 35mm dish in duplicate.
- Culture & Scoring: Place dishes in a humidified incubator at 37°C, 5% CO2 for 14-16 days. Score colonies (CFU-GEMM, BFU-E, CFU-GM) under an inverted microscope. Compare colony number and type to an unedited control.
Protocol 3.4:In VivoEngraftment & Multi-Lineage Potential Assay (NSG Mouse Model)
Objective: Gold-standard assessment of long-term HSC function.
- Mouse Conditioning: Irradiate 8-12 week old NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mice with a split dose of 275 cGy, 4 hours apart.
- Cell Transplantation: Within 24 hours of irradiation, inject 2-5 x 10^5 human CD34+ cells (edited or control) via tail vein in 200 µL of PBS + 1% HSA. Include a non-injected control.
- Monitoring: At 8, 12, and 16 weeks post-transplant, collect peripheral blood via retro-orbital bleed. Lyse red blood cells and stain for human CD45 to assess overall engraftment.
- Terminal Analysis: At 16 weeks, euthanize mice. Harvest bone marrow (femurs, tibiae), spleen, and thymus. Process into single-cell suspensions.
- Flow Cytometry: Stain cells with antibodies for human CD45, CD33 (myeloid), CD19 (B lymphoid), and CD34/CD38 (progenitors). Analyze on a flow cytometer.
- Genomic Analysis: Isolve genomic DNA from bone marrow. Use ddPCR or NGS to quantify the frequency of edited BCL11A alleles in engrafted human cells.
Diagrams & Visualizations
Diagram Title: Exa-Cel HSC Editing & Engraftment QC Workflow
Diagram Title: Key Stressors & Interventions for HSC Engraftment
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Reagents for HSC Editing & Engraftment Studies
| Reagent / Solution | Function / Purpose | Example Product / Component |
|---|---|---|
| Stem Cell Mobilization Cocktail | Induces HSC egress from bone marrow for collection. | G-CSF (Filgrastim), Plerixafor (AMD3100) |
| Clinical-Grade CD34+ Selection Kit | Immunomagnetic positive selection of target HSC population. | CliniMACS CD34 Reagent & Instrument |
| Serum-Free Expansion Medium | Supports HSC survival and maintenance ex vivo with minimal differentiation. | X-VIVO 15, StemSpan SFEM II |
| Early-Acting Cytokine Cocktail | Promotes HSC survival, priming, and maintains stemness during culture. | Recombinant human SCF, TPO, FLT3-Ligand |
| Small Molecule Stemness Enhancer | Aryl hydrocarbon receptor antagonist; suppresses differentiation. | StemRegenin 1 (SR1) |
| High-Fidelity Cas9 Protein | CRISPR nuclease with reduced off-target activity for therapeutic editing. | HiFi Cas9, Alt-R S.p. HiFi Cas9 Nuclease V3 |
| Chemically Modified sgRNA | Enhances stability and reduces immunogenicity of guide RNA. | Alt-R CRISPR-Cas9 sgRNA with 2'-O-methyl analogs |
| Primary Cell Electroporation System | Enables high-efficiency, low-toxicity delivery of RNP into sensitive HSCs. | Lonza 4D-Nucleofector System with P3 Kit |
| Methylcellulose CFU Assay Medium | Semi-solid medium to quantify clonogenic progenitor potential. | MethoCult H4435 Enriched |
| Immunodeficient Mouse Model | In vivo model for assessing human HSC homing and long-term engraftment. | NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) |
| Multiparameter Flow Cytometry Panels | For phenotyping HSCs (CD34, CD38, CD90, CD45RA) and lineage analysis. | Antibodies against human CD45, CD34, CD19, CD33, etc. |
Application Notes on Scalability Challenges
Scaling the manufacturing of exagamglogene autotemcel (exa-cel) from clinical to commercial phases presents distinct challenges that require proactive planning. The core process involves editing patient-derived CD34+ hematopoietic stem and progenitor cells (HSPCs) via CRISPR-Cas9 to disrupt the erythroid-specific enhancer of the BCL11A gene, thereby inducing fetal hemoglobin (HbF) production. Scalability directly impacts critical quality attributes (CQAs), including editing efficiency, viability, potency, and purity.
Key Scalability Considerations:
- Starting Material: Consistency in leukapheresis product collection, shipment, and CD34+ cell selection across global collection centers.
- Vector and Reagents: Transition from research-grade to clinical and commercial-grade CRISPR-Cas9 ribonucleoprotein (RNP) complex and ancillary reagents under strict quality control.
- Process Parameters: Maintaining optimal cell density, electroporation conditions (voltage, pulse length), and expansion dynamics during scale-out.
- Facility Design: Implementing closed, automated systems to reduce operator-dependent variability and contamination risk.
- Analytical Testing: Scaling QC methods (e.g., NGS for on-target editing, off-target analysis, ddPCR for HbF) for higher throughput with validated, transferable assays.
Table 1: Representative Scale-Up Parameters for Exa-Cel Manufacturing
| Process Parameter | Phase I/II (Clinical) | Phase III/Commercial (Target) | Critical Impact on CQA |
|---|---|---|---|
| Batch Size (CD34+ cells) | 1-5 x 10^8 | 1-2 x 10^9 | Final cell dose, process robustness |
| Electroporation Runs | Multiple, sequential | Single, scaled-up or parallelized | Editing efficiency uniformity, viability |
| Culture Duration | 6-10 days | Optimized to ≤ 7 days | Cell potency, differentiation risk |
| Final Formulation Volume | ~100 mL | Minimized, consistent | Cryopreservation efficiency, storage |
| Release Testing Turnaround | 10-14 days | < 7 days (via rapid assays) | Product shelf-life, patient scheduling |
GMP Compliance Protocol Framework
This protocol outlines the core GMP-compliant manufacturing steps for exa-cel, emphasizing points critical for regulatory compliance and commercial supply.
Objective: To manufacture an autologous, gene-edited CD34+ HSPC product for the treatment of transfusion-dependent beta-thalassemia and sickle cell disease, meeting pre-defined CQAs and regulatory specifications.
Materials & Reagents (Research Reagent Solutions Toolkit):
Table 2: Essential Materials for GMP-Compliant Exa-Cel Manufacturing
| Item | Function | Critical Quality Attribute |
|---|---|---|
| CliniMACS CD34 Reagent System | Immunomagnetic selection of CD34+ cells from leukapheresis. | Purity, viability, recovery. |
| GMP-grade CRISPR-Cas9 RNP | Pre-complexed guide RNA targeting the BCL11A enhancer and Cas9 protein. | Editing efficiency, sterility, endotoxin levels. |
| Electroporation System (e.g., MaxCyte GT/ATE) | Enables delivery of RNP into CD34+ cells via electroporation. | Viability, editing efficiency, scalability. |
| Serum-free, Xeno-free Media (e.g., StemSpan) | Supports the expansion and maintenance of HSPCs during culture. | Supports cell growth, maintains stemness. |
| Cryopreservation Solution (e.g., CryoStor) | Formulates final product for controlled-rate freezing and storage. | Post-thaw viability and recovery. |
| MycoAlert Detection Kit | Rapid mycoplasma testing of in-process and final product. | Sterility assurance. |
Detailed Protocol:
Step 1: Receipt and Processing of Apheresis Material
- Receive patient leukapheresis unit at the manufacturing facility under controlled temperature conditions.
- Perform identity testing and confirm donor-recipient chain of custody.
- Isolate CD34+ cells using a closed, automated system (e.g., CliniMACS Prodigy) according to validated SOPs. Record cell count, viability (≥ 90%), and purity (≥ 80% CD34+).
Step 2: Pre-stimulation and Gene Editing
- Resuspend selected CD34+ cells in pre-warmed, cytokine-supplemented serum-free media at a defined density (e.g., 1x10^6 cells/mL).
- Incubate cells for 18-24 hours at 37°C, 5% CO2.
- Prepare the GMP-grade BCL11A-targeting RNP complex per manufacturer's instructions.
- Wash and resuspend pre-stimulated cells in electroporation buffer.
- Combine cells with RNP and electroporate using a validated, scalable protocol (e.g., MaxCyte ATE, OC-100 protocol). Include process controls (non-electroporated, mock-electroporated).
Step 3: Post-Editing Culture and Expansion
- Immediately transfer electroporated cells to recovery media, then to expansion media.
- Culture cells in a controlled bioreactor or culture bags for a defined period (target ≤ 7 days).
- Monitor cell density, viability, and metabolites (glucose, lactate) daily. Maintain cell density within the validated range.
Step 4: Formulation, Cryopreservation, and Release
- Harvest cells, perform final wash, and resuspend in cryopreservation medium.
- Fill final product into cryobags, label, and initiate controlled-rate freezing.
- Transfer cryobags to vapor-phase liquid nitrogen for long-term storage.
- Perform full suite of release tests on an aliquot: sterility, mycoplasma, endotoxin, viability, identity (CD34+%), editing efficiency (NGS), potency (colony-forming unit assay with HbF expression), and vector clearance (if applicable).
Visualized Workflows and Pathways
Exa-Cel GMP Manufacturing Process Flow
BCL11A Editing Leads to HbF Re-expression
Clinical Efficacy, Safety, and Competitive Analysis of Exa-cel
Article
Within the paradigm of genetic therapies for hemoglobinopathies, the development of exagamglogene autotemcel (exa-cel), an autologous CD34+ cell therapy utilizing CRISPR-Cas9 to edit the erythroid-specific enhancer of BCL11A, represents a pivotal advancement. The therapeutic thesis posits that disruption of this enhancer reduces BCL11A expression, thereby de-repressing fetal hemoglobin (HbF) production in red blood cells. This induction of HbF is hypothesized to compensate for the defective adult hemoglobin in sickle cell disease (SCD) and transfusion-dependent beta-thalassemia (TDT), addressing the root pathophysiology. The clinical validation of this protocol is demonstrated in the pivotal Phase 3 trials CLIMB SCD-121 (for SCD) and CLIMB THALES (for TDT). This application note details the experimental outcomes and associated research methodologies central to validating the exa-cel BCL11A enhancer editing paradigm.
Table 1: Primary Efficacy Endpoints from Pivotal Phase 3 Trials
| Trial (Condition) | Primary Endpoint | Timepoint | Result (n/N; %) | 95% CI |
|---|---|---|---|---|
| CLIMB SCD-121 (Severe Sickle Cell Disease) | Freedom from severe Vaso-Occlusive Crises (VOCs) | Month 12 through Month 24 | 29/32 (90.6%) | (75.8%, 97.1%) |
| CLIMB THALES (Transfusion-Dependent Beta-Thalassemia) | Transfusion Independence (sustained weighted average Hb ≥9 g/dL without RBC transfusions) | Month 12 through Month 24 | 31/32 (96.9%) | (84.3%, 99.9%) |
Table 2: Key Hematological and Molecular Biomarkers (Follow-up Data)
| Parameter | Trial | Baseline Mean (SD) | Post-Treatment Mean (SD) | Notes |
|---|---|---|---|---|
| HbF (%) | SCD-121 | <10% | >40% (Month 12+) | Associated with VOC elimination |
| HbF (g/dL) | THALES | <2 g/dL | >10 g/dL (Month 12+) | Sufficient to eliminate transfusion need |
| Total Hemoglobin (g/dL) | SCD-121 | ~8.5 g/dL | >11 g/dL (Month 12+) | Resolution of anemia |
| Allelic Editing Efficiency | Both | 0% | ~70-80% (in engrafted cells) | Measured in peripheral blood mononuclear cells |
| BCL11A Expression (Erythroid Lineage) | Both | 100% (reference) | ~20-30% of baseline | Quantified via qRT-PCR in differentiated progenitors |
Experimental Protocols for Efficacy Validation
Protocol A: Assessment of BCL11A Enhancer Editing Efficiency & Indel Spectrum Objective: Quantify the frequency and characterize the nature of CRISPR-Cas9-induced insertions/deletions (indels) at the BCL11A erythroid enhancer target site in post-infusion patient samples. Materials: Genomic DNA from peripheral blood CD34+ or mononuclear cells, PCR primers flanking the target site, NGS library prep kit, bioinformatics pipeline (e.g., CRISPResso2). Procedure: 1. Isolate genomic DNA from patient blood samples at sequential time points (e.g., Month 3, 6, 12, 24). 2. Amplify the target genomic region by PCR. 3. Prepare next-generation sequencing (NGS) libraries and perform deep sequencing (≥10,000x coverage). 4. Analyze sequencing data using a validated bioinformatics tool to calculate the percentage of reads with indels at the target site (editing efficiency) and classify the specific indel sequences. Output: Table of editing percentages and indel distribution profile per sample.
Protocol B: Quantification of Fetal Hemoglobin (HbF) in Peripheral Erythrocytes Objective: Measure the percentage and concentration of HbF in total hemoglobin post-treatment. Materials: Peripheral whole blood, HPLC system with cation-exchange column or capillary electrophoresis instrument. Procedure: 1. Prepare hemolysate from EDTA-anticoagulated patient blood. 2. Inject hemolysate into the HPLC or capillary electrophoresis system calibrated with hemoglobin controls (HbA, HbF, HbA2, HbS). 3. Separate hemoglobins based on charge/size. Identify and integrate peaks corresponding to HbF. 4. Calculate %HbF (peak area HbF / total hemoglobin peak area) and absolute HbF (g/dL) = (Total Hb in g/dL) * (%HbF/100). Output: Time-series data of %HbF and HbF g/dL correlated with clinical endpoints.
Protocol C: In Vitro Erythroid Differentiation for BCL11A Expression Analysis Objective: Evaluate functional consequence of editing on BCL11A protein downregulation in the erythroid lineage. Materials: Post-infusion CD34+ cells, serum-free erythroid differentiation media (with SCF, EPO, IL-3, dexamethasone), antibodies for flow cytometry (CD235a, CD71), intracellular staining antibodies for BCL11A. Procedure: 1. Culture isolated CD34+ cells in a three-phase erythroid differentiation protocol over ~18 days. 2. Harvest cells at defined progenitor (burst-forming unit-erythroid, BFU-E) and later (orthochromatic erythroblast) stages. 3. Perform intracellular staining for BCL11A protein and surface staining for erythroid markers. 4. Analyze by flow cytometry to determine mean fluorescence intensity (MFI) of BCL11A in the edited (e.g., CD235a+) erythroid population compared to isotype control. Output: Flow cytometry histograms and quantitative MFI reduction data confirming mechanistic target engagement.
Pathway and Workflow Visualizations
Title: Exa-cel Manufacturing and Therapeutic Mechanism
Title: Molecular Pathway from BCL11A Edit to Clinical Benefit
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function in exa-cel / BCL11A Research |
|---|---|
| CRISPR-Cas9 Ribonucleoprotein (RNP) | Pre-complexed guide RNA (targeting BCL11A +13 enhancer) and Cas9 protein. Enables efficient, transient editing of CD34+ HSPCs with reduced off-target risk. |
| GMP-grade StemSpan SFEM II | Serum-free, cytokine-supported medium essential for the maintenance and viability of hematopoietic stem cells during the ex vivo editing and expansion process. |
| Recombinant Human Cytokines (SCF, TPO, FLT-3L) | Critical growth factors added to culture media to promote HSPC survival and proliferation during manufacturing without driving differentiation. |
| CliniMACS CD34 Reagent System | Magnetic bead-based selection system for the isolation of high-purity CD34+ cells from leukapheresis product, a critical initial manufacturing step. |
| Droplet Digital PCR (ddPCR) Assays | For precise, absolute quantification of editing efficiency and vector copy number without reliance on standard curves, crucial for potency and safety testing. |
| HBG1/HBG2-specific qPCR Primers | To quantitatively measure the reactivation of fetal globin mRNA transcripts in differentiated erythroid cells, a key pharmacodynamic biomarker. |
| Anti-BCL11A (XL) Antibody | For Western blot or intracellular flow cytometry to confirm downregulation of the BCL11A protein (particularly the XL isoform) in the erythroid lineage post-editing. |
| Next-Generation Sequencing (NGS) Panel | Targeted panel for deep sequencing of the on-target site (indel analysis) and predicted off-target sites to comprehensively assess editing specificity. |
Application Notes
The development of exagamglogene autotemcel (exa-cel), an autologous CRISPR-Cas9-edited cell therapy targeting the BCL11A erythroid enhancer for the treatment of sickle cell disease and β-thalassemia, necessitates a rigorous and multifaceted safety assessment. This framework focuses on three critical, interlinked safety axes: Genotoxicity, Insertion/Deletion (InDel) patterns at the on-target site, and the potential for Clonal Hematopoiesis (CH). The central thesis posits that a comprehensive safety profile for BCL11A enhancer editing is not defined by a single metric but by the integrated analysis of these factors, ensuring that high-efficacy editing does not come at the cost of genomic instability or pre-malignant clonal expansion.
1. Genotoxicity Analysis: Off-target editing remains a primary theoretical risk for CRISPR-based therapies. For exa-cel, a tailored analysis strategy is employed:
- In silico Prediction: Initial bioinformatic screening identifies potential off-target sites with high sequence homology to the single guide RNA (sgRNA) targeting the BCL11A enhancer, allowing for mismatches and bulges.
- Cell-Based Assays: Primary human CD34+ hematopoietic stem and progenitor cells (HSPCs) are edited using the clinical manufacturing process. Subsequent assays include:
- Circularization for In Vitro Reporting of Cleavage Effects by Sequencing (CIRCLE-seq): An in vitro, amplification-free method that uses purified genomic DNA from edited cells to comprehensively identify nuclease-induced double-strand breaks across the genome.
- Targeted Next-Generation Sequencing (NGS): Deep sequencing of the top-ranked in silico and CIRCLE-seq identified loci in pre- and post-edit product samples.
- Unbiased Genome-Wide Assays: Techniques like GUIDE-seq or DISCOVER-seq may be employed in research settings to provide orthogonal, unbiased confirmation of off-target profile.
2. InDel Pattern Analysis: The distribution of DNA repair outcomes at the on-target locus directly influences both therapeutic efficacy (disruption of the BCL11A enhancer) and potential genotoxicity (creation of pathogenic sequences).
- High-Throughput Sequencing: Amplicon-based NGS of the edited genomic region in the final drug product and post-infusion patient samples.
- Bioinformatic Deconvolution: Sequences are analyzed to categorize InDels by type (e.g., -1bp, -2bp, +1bp, large deletions, complex patterns) and frequency.
- Safety Correlation: The distribution is monitored for the absence of high-frequency, long-range deletions or genomic rearrangements that could impair the function of adjacent genes or regulatory elements.
3. Clonal Hematopoiesis Analysis: The ex vivo culture and editing process imposes selective pressures. Monitoring for CH is critical to assess whether the process inadvertently promotes the expansion of clones bearing mutations in genes associated with hematological malignancies (e.g., DNMT3A, TET2, ASXL1).
- Error-Corrected NGS: Ultra-deep sequencing (e.g., >10,000x coverage) using duplex sequencing methods on pre-manufacture apheresis and post-edit drug product samples to identify and quantify very low-frequency variants in a panel of CH-associated genes.
- Longitudinal Tracking: Monitoring variant allele frequencies (VAFs) of any detected CH mutations in patient blood samples over time post-infusion to distinguish pre-existing, stable CH from editing-process-related clonal expansion.
Integrated Risk Assessment: The final safety assessment is integrative. A clean off-target profile, a predictable on-target InDel pattern dominated by small frameshift deletions, and the absence of newly emergent or expanding CH clones collectively support a favorable safety profile for the BCL11A enhancer editing protocol.
Experimental Protocols
Protocol 1: CIRCLE-seq for Unbiased Off-Target Cleavage Detection
Objective: To identify potential CRISPR-Cas9 off-target sites genome-wide in an in vitro system using genomic DNA from exa-cel-edited CD34+ cells.
Materials:
- Purified genomic DNA (gDNA) from edited and control HSPCs.
- CIRCLE-seq kit or components: Circligase, exonuclease mix, phi29 polymerase, in vitro transcription reagents.
- Cas9 protein and target sgRNA.
- NGS library preparation kit.
- Bioinformatics pipeline (BLAT, BWA, custom scripts).
Procedure:
- DNA Shearing & End-Repair: Fragment 2 µg of gDNA to ~300bp using a sonicator. Repair ends to be blunt, phosphorylated.
- Circularization: Perform intramolecular circularization of fragments using Circligase. This step removes free ends, preventing artifact generation.
- Digestion of Linear DNA: Treat with exonuclease to degrade any remaining linear DNA, enriching for circularized molecules.
- In Vitro Cleavage: Incubate purified circular DNA with Cas9 ribonucleoprotein (RNP) complex (Cas9 + sgRNA) to cleave at genomic sites complementary to the sgRNA.
- Linearization & Adapter Ligation: Re-linearize the nicked circles. Ligate sequencing adapters to the new ends created by Cas9 cleavage.
- Amplification & Sequencing: Amplify adapter-ligated fragments by PCR and subject to high-throughput sequencing.
- Bioinformatic Analysis: Map sequencing reads to the reference genome. Identify sites of enrichment in the Cas9-treated sample versus control. Rank sites by read count.
Protocol 2: On-Target InDel Pattern Analysis by Amplicon Sequencing
Objective: To characterize the spectrum and frequency of insertion and deletion mutations at the BCL11A enhancer target site in the final drug product.
Materials:
- Genomic DNA from drug product aliquot.
- High-fidelity PCR polymerase.
- PCR primers flanking the cut site (amplicon ~300-400bp).
- NGS index adapters.
- MiSeq or similar sequencing platform.
- Analysis software (CRISPResso2, Geneious).
Procedure:
- Amplicon PCR: Amplify the target locus from 100ng of gDNA using barcoded primers.
- NGS Library Preparation: Purify PCR products and perform a second, limited-cycle PCR to add full Illumina sequencing adapters and sample-specific dual indices.
- Pooling & Sequencing: Quantify libraries, pool equimolarly, and sequence on a MiSeq system (2x300bp paired-end recommended for accuracy).
- Sequence Analysis:
- Demultiplex reads and merge paired ends.
- Align reads to the reference BCL11A enhancer sequence.
- Use CRISPResso2 to quantify the percentage of aligned reads containing insertions, deletions, or substitutions within a window around the expected cut site.
- Categorize and plot the frequency of each unique InDel variant.
Protocol 3: Surveillance of Clonal Hematopoiesis by Duplex Sequencing
Objective: To detect low-frequency somatic mutations in CH-associated genes in pre-apheresis and post-edit drug product samples.
Materials:
- High-quality gDNA (>500ng) from pre- and post-edit samples.
- Custom hybridization capture panel targeting exons of DNMT3A, TET2, ASXL1, TP53, JAK2, etc.
- Duplex sequencing adapter kit.
- High-fidelity PCR enzymes.
- Illumina sequencing platform.
Procedure:
- Duplex Adapter Ligation: Ligate special double-stranded adapters containing random molecular barcodes to sheared gDNA. Each original DNA molecule receives a unique tag.
- Hybrid Capture: Enrich for target genes using biotinylated probes and streptavidin beads.
- Library Amplification & Sequencing: Amplify the captured library and sequence to ultra-high depth (>10,000x raw coverage).
- Error-Corrected Analysis:
- Group sequencing reads derived from the same original DNA molecule using the molecular barcode.
- Generate a consensus sequence for each original molecule, eliminating PCR and sequencing errors.
- Call variants by comparing consensus sequences to the reference genome.
- Report variants with a VAF as low as 0.1% with high confidence. Track specific mutations and their VAFs across time points.
Data Tables
Table 1: Summary of Off-Target Analysis for BCL11A Enhancer sgRNA
| Analysis Method | Potential Off-Target Sites Identified | Sites Validated in Edited HSPCs (NGS) | Highest Indel Frequency at Validated Site |
|---|---|---|---|
| In Silico Prediction | 15-25 | 0-2 | <0.1% |
| CIRCLE-seq In Vitro | 5-15 | 0-1 | <0.05% |
| Unbiased In Situ (e.g., GUIDE-seq) | 0-5 | 0 | Not Detected |
Table 2: Typical On-Target InDel Pattern in Exa-Cel Drug Product
| InDel Category | Example | Frequency Range | Functional Consequence (Enhancer Disruption) |
|---|---|---|---|
| -1 bp Deletion | ΔT | 40-60% | High (Frameshift) |
| -2 bp Deletion | ΔGA | 10-20% | High (Frameshift) |
| +1 bp Insertion | +A | 5-15% | High (Frameshift) |
| Other Small InDels (-5 to +5 bp) | Various | 10-20% | Variable |
| Large Deletions (>20 bp) | - | <0.5% | Assessed Individually |
Table 3: Clonal Hematopoiesis Mutation Surveillance
| Sample Type | Prevalence of CH Mutations (VAF > 0.5%) | Most Frequently Altered Gene | Typical Longitudinal Trend Post-Infusion |
|---|---|---|---|
| Pre-Apheresis (Patient Baseline) | ~5-10% (age-dependent) | DNMT3A | Stable or declining VAF |
| Post-Edit Drug Product | No new mutations attributed to process | - | - |
| Patient Follow-up (6-24 Months) | No consistent expansion of pre-existing clones | - | - |
Visualizations
Title: Integrated Safety Analysis Framework
Title: CIRCLE-seq Off-Target Detection Workflow
Title: On-Target InDel Pattern Analysis Protocol
The Scientist's Toolkit
Table 4: Key Research Reagent Solutions for Safety Profiling
| Item | Function in Analysis | Specific Example / Note |
|---|---|---|
| Primary Human CD34+ HSPCs | The biologically relevant cell substrate for all ex vivo editing and safety assays. Crucial for measuring off-targets in the correct genomic and epigenetic context. | Mobilized peripheral blood or cord blood derived. |
| Clinical-Grade Cas9 Protein & sgRNA | The active editing components. Using the exact RNP formulation intended for therapy ensures assay relevance. | Recombinant high-purity S. pyogenes Cas9, synthetic sgRNA. |
| CIRCLE-seq Kit | Provides optimized enzymes and buffers for the unbiased, in vitro genome-wide identification of nuclease cleavage sites. | Commercial kit or lab-built component set. |
| Duplex Sequencing Adapter Kit | Contains unique molecular barcodes and adapters essential for error-corrected, ultra-sensitive mutation detection. | Kits from specialized NGS providers. |
| Hybridization Capture Panel (CH Genes) | Biotinylated oligonucleotide probes designed to enrich sequences from a defined panel of clonal hematopoiesis and leukemia-associated genes prior to sequencing. | Custom or pan-cancer focused panels. |
| High-Fidelity PCR Polymerase | Essential for accurate, low-error amplification of target loci for both InDel and CH sequencing libraries to prevent introduction of artifacts. | Enzymes like Q5, KAPA HiFi. |
| CRISPResso2 Software | The standard bioinformatics tool for quantifying genome editing outcomes from NGS data. Precisely calculates InDel percentages and patterns. | Open-source, web-based or command line. |
| Ultra-High-Throughput Sequencer | Platform capable of generating the massive sequencing depth required for duplex sequencing and high-sensitivity variant detection. | Illumina NovaSeq, PacBio Revio. |
Comparison with Lentiviral Gene Therapy (e.g., lovotibeglogene autotemcel/lovo-cel)
This application note provides a detailed comparison between exagamglogene autotemcel (exa-cel), a CRISPR-Cas9-based therapy targeting the BCL11A erythroid-specific enhancer for β-hemoglobinopathies, and lovotibeglogene autotemcel (lovo-cel), an LentiVector-based β-globin gene addition therapy. The context is a thesis on optimizing the BCL11A enhancer editing protocol, necessitating a clear understanding of the mechanistic, manufacturing, and clinical distinctions between these two advanced therapeutic modalities.
Table 1: Fundamental Therapeutic Characteristics
| Feature | Exagamglogene Autotemcel (exa-cel) | Lovotibeglogene Autotemcel (lovo-cel) |
|---|---|---|
| Therapeutic Platform | CRISPR-Cas9 Gene Editing | Lentiviral Vector Gene Addition |
| Genetic Target | BCL11A Erythroid Enhancer | β-globin Gene (HBB) |
| Mechanism of Action | Disruption of enhancer to reduce BCL11A, inducing fetal hemoglobin (HbF) | Addition of a functional β-globin transgene (β^A-T87Q) |
| Key Components | sgRNA, Cas9 nuclease, Electroporation | VSV-G pseudotyped Lentiviral Vector |
| Integration Profile | No exogenous DNA integration; on/off-target edits at DNA break sites | Semi-random genomic integration of provirus |
| Manufacturing Complexity | High (cell isolation, editing, expansion) | High (cell isolation, transduction, expansion) |
| Clinical Status (as of 2024) | Approved in US/UK/EU for SCD & TDT | Under regulatory review for SCD |
Table 2: Key Clinical Efficacy & Safety Metrics (Representative Data)
| Parameter | exa-cel (CLIMB-111/121) | lovo-cel (Phase 1/2 HGB-206) |
|---|---|---|
| Patients (n) | >50 TDT/SCD | ~35 SCD |
| Follow-up Duration | Up to 48 months | Up to 60 months |
| HbF Induction | >40% of total Hb, pancellular | ~40% of total Hb, pancellular |
| VOC Resolution (SCD) | >95% patients free | >90% patients free |
| Vector Copy Number/Edit Rate | N/A (editing efficiency >90%) | VCN: ~2-4 copies/diploid genome |
| Genotoxicity Events | None reported to date | None reported to date |
| Common AEs | Cytopenias from conditioning, HSCT-related | Cytopenias from conditioning, HSCT-related |
Detailed Experimental Protocols
Protocol 1: BCL11A Enhancer Editing & Analysis (exa-cel Workflow)
Objective: To isolate CD34+ HSPCs, perform CRISPR-Cas9 editing of the BCL11A enhancer, and quantify editing efficiency and HbF induction potential.
Materials: See "Scientist's Toolkit" below. Procedure:
- Mobilization & Apheresis: Collect hematopoietic stem and progenitor cells (HSPCs) from patient via mobilization and apheresis.
- CD34+ Cell Selection: Isolate CD34+ cells using clinical-grade immunomagnetic selection (e.g., CliniMACS). Assess viability and purity (flow cytometry).
- CRISPR-Cas9 Electroporation: a. Pre-stimulate cells in serum-free medium containing SCF, TPO, FLT3-L for 24-48h. b. Formulate ribonucleoprotein (RNP) complex: Combine purified Cas9 protein (100 µg/mL final) with synthetic sgRNA targeting the BCL11A enhancer (e.g., sequence: GACAGATCAGAGACACTGCGAGG) at a 1:2 molar ratio. Incubate 10 min at room temperature. c. Electroporate 1-5 x 10^6 CD34+ cells/mL with the RNP complex using a 4D-Nucleofector (pulse code EO-115) in P3 buffer.
- Post-Editing Culture: Immediately transfer cells to recovery medium with cytokines. Culture for 48-72h for initial analysis or proceed to expansion/differentiation.
- Editing Efficiency Assessment: a. INDEL Frequency: At day 3, extract genomic DNA. Perform PCR amplification of the on-target region. Use TIDE (Tracking of Indels by Decomposition) or NGS to quantify insertion/deletion rates. Target: >80% editing. b. On/Off-Target Analysis: Perform GUIDE-seq or CAST-Seq on a sample to profile genome-wide editing events.
- Functional Potency Assay (Erythroid Differentiation): a. Culture edited CD34+ cells in a three-phase erythroid differentiation medium (SCF, EPO, IL-3, steroids). b. At day 18-21, harvest erythroblasts. Perform flow cytometry for HbF (F-cells) using HbF antibody staining and measure HbF% by HPLC. Target: >40% F-cells.
Protocol 2: Lentiviral Transduction & Analysis (lovo-cel Workflow)
Objective: To transduce CD34+ HSPCs with a lentiviral vector encoding β^A-T87Q-globin and assess transduction efficiency and transgene expression.
Procedure:
- Cell Collection & Selection: Perform Steps 1 & 2 from Protocol 1.
- Pre-stimulation: Culture CD34+ cells in X-VIVO 10 medium with SCF, TPO, FLT3-L (100 ng/mL each) for 24h.
- Lentiviral Transduction: a. Pre-load RetroNectin (20 µg/cm²) onto non-tissue culture treated plates. b. Resuspend pre-stimulated cells at 1 x 10^6 cells/mL in fresh medium with same cytokines and protamine sulfate (4 µg/mL). c. Add clinical-grade LVV encoding β^A-T87Q-globin at a target MOI of 5-10. Centrifuge (1000g, 90 min, 32°C) for spinoculation. d. Incubate at 37°C for 16-24h. e. Repeat transduction with fresh vector supernatant.
- Post-Transduction Culture: Wash cells and continue culture in cytokine-containing medium for expansion.
- Transduction Efficiency Assessment: a. Vector Copy Number (VCN): At day 7, extract genomic DNA. Perform ddPCR using primers/probes specific to the vector backbone (e.g., WPRE) and a reference gene (e.g., RPP30). Calculate average VCN per diploid genome. Target range: 2-4. b. Transduction Efficiency: Perform flow cytometry for a surface marker (if included) or by qPCR for vector-specific RNA.
- Globin Expression Analysis (Erythroid Differentiation): a. Differentiate transduced CD34+ cells as in Protocol 1, Step 6. b. Analyze hemolysates by HPLC/CE to quantify expression of β^A-T87Q-globin (distinct retention time) and total HbF. Assess % of anti-sickling hemoglobin (HbA^T87Q + HbF).
Visualization Diagrams
Diagram Title: Gene Therapy Mechanisms: Editing vs. Addition
Diagram Title: Comparative Manufacturing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for BCL11A/Globin Gene Therapy Research
| Reagent/Material | Function & Specification | Example Product/Catalog |
|---|---|---|
| Immunomagnetic CD34+ Selection Kit | Isolation of pure HSPC population from apheresis product. Critical for process purity. | Miltenyi Biotec CliniMACS CD34 Reagent |
| GMP-grade Cytokines (SCF, TPO, FLT3-Ligand) | Pre-stimulation of HSPCs to prime for editing/transduction. Must be xeno-free. | PeproTech (GMP Grade) |
| Cas9 Nuclease, HiFi or WT | High-specificity nuclease for gene editing. HiFi variants reduce off-targets. | IDT Alt-R HiFi Cas9 |
| Chemically Modified sgRNA | Targets BCL11A erythroid enhancer. Modifications (2'-O-methyl, phosphorothioate) enhance stability. | Synthego (CRISPRevolution sgRNA EZ Kit) |
| 4D-Nucleofector System & Kit | Device and optimized buffer for efficient RNP delivery into primary CD34+ cells. | Lonza 4D-Nucleofector, P3 Primary Cell Kit |
| Clinical-grade Lentiviral Vector | VSV-G pseudotyped LVV encoding β^A-T87Q-globin. Titer >1e8 IU/mL. | Produced under GMP (e.g., Oxford Biomedica) |
| RetroNectin | Recombinant fibronectin fragment. Enhances lentiviral transduction by co-localizing cells and virus. | Takara Bio (RetroNectin) |
| Vector Copy Number Assay | ddPCR assay for precise quantification of integrated LVV copies per genome. | Bio-Rad ddPCR Supermix for Probes (no dUTP) |
| Erythroid Differentiation Media Kit | Serum-free, staged media for robust in vitro differentiation of CD34+ cells to erythroblasts. | STEMCELL Technologies (StemSpan Erythroid Expansion) |
| HbF Flow Cytometry Kit | Antibody-based intracellular staining for HbF to quantify F-cells post-differentiation. | BD Pharmingen Anti-HbF-PE |
| HPLC System for Hemoglobin | Analytical system for separation and quantification of hemoglobin variants (HbA, HbS, HbF, HbA^T87Q). | Tosoh HLC-723 G11 |
| Next-Gen Sequencing Kit | For comprehensive on/off-target analysis (e.g., GUIDE-seq, CAST-Seq, or targeted amplicon-seq). | Illumina MiSeq, CAST-Seq Kit (Eurofins) |
Positioning vs. Allogeneic Hematopoietic Stem Cell Transplantation (allo-HSCT)
The therapeutic landscape for severe hemoglobinopathies, particularly sickle cell disease (SCD) and β-thalassemia, is being redefined by the emergence of autologous gene-editing therapies. Research within the thesis on exagamglogene autotemcel (exa-cel)—an investigational therapy involving CRISPR-Cas9 editing of the BCL11A erythroid-specific enhancer in a patient's own hematopoietic stem and progenitor cells (HSPCs)—necessitates a clear comparison against the historical standard of care, allo-HSCT. This analysis positions exa-cel not as a universal replacement, but as a complementary modality with distinct risk-benefit profiles, patient eligibility considerations, and mechanistic implications. The protocol development for exa-cel production directly parallels and diverges from established allo-HSCT workflows, focusing on autologous cell processing, ex vivo editing, and manufacturing consistency versus donor matching, graft engineering, and immunosuppression.
Comparative Data Analysis: exa-cel vs. Allo-HSCT
Table 1: Key Efficacy and Safety Outcomes
| Parameter | Exagamglogene Autotemcel (exa-cel) | Allogeneic HSCT (Matched Sibling Donor) | Allogeneic HSCT (Unrelated/Mismatched Donor) |
|---|---|---|---|
| Source of Graft | Autologous (patient's own CD34+ cells) | Allogeneic (sibling donor) | Allogeneic (unrelated or haploidentical donor) |
| Primary Efficacy Endpoint (SCD) | Freedom from severe vaso-occlusive crises (≥12 months) | Event-free survival (graft survival without complications) | Event-free survival |
| Reported Efficacy (Recent Trials) | ~96% (CLIMB SCD-121, 24-mo median f/u) | >90% (long-term EFS with MSD) | 80-90% (matched unrelated); 70-85% (haploidentical) |
| Key Acute Risks | Myeloablative conditioning toxicity, insertional mutagenesis (theoretical), off-target editing | Graft-versus-host disease (GvHD), regimen-related toxicity, graft failure, infection | Higher risk of GvHD, graft failure, infection, transplant-related mortality |
| Key Chronic Risks | Potential for clonal dominance, unknown long-term effects of editing | Chronic GvHD, long-term immunosuppression, endocrine dysfunction, secondary malignancies | Higher incidence and severity of chronic GvHD |
| Need for Immunosuppression | No (autologous graft) | Yes, prolonged (to prevent/treat GvHD) | Yes, more intensive and prolonged |
| Time to Immune Reconstitution | ~4-6 weeks post-infusion | 6-12+ months (delayed by immunosuppression) | Often longer, higher infection risk |
Table 2: Logistical and Patient Selection Factors
| Factor | Exagamglogene Autotemcel (exa-cel) | Allogeneic HSCT |
|---|---|---|
| Donor Requirement | None | Critical barrier; only ~20-30% have MSD |
| Manufacturing Time | ~4-6 months from apheresis to infusion | Variable, depends on donor workup/availability |
| Conditioning Regimen | Myeloablative (e.g., busulfan) required | Myeloablative or reduced-intensity |
| Impact of Prior Therapy | Requires adequate CD34+ collection; prior transfusion history may affect yield | Can be complicated by alloimmunization from transfusions |
| Age Considerations | Initially adults, expanding to pediatric (≥12 years in trials) | Standard for pediatric patients with MSD; age increases risk in adults |
| Cost & Infrastructure | Extremely high (one-time); requires specialized GMP manufacturing center | Very high; requires donor registries, HLA labs, and transplant centers |
Experimental Protocols
Protocol 1:BCL11AEnhancer Editing & exa-cel Product Characterization
This protocol outlines key validation steps for the edited CD34+ cell product.
- CD34+ HSPC Mobilization, Apheresis, and Selection: Mobilize with granulocyte colony-stimulating factor (G-CSF) and plerixafor. Perform apheresis to collect mononuclear cells. Isulate CD34+ cells via immunomagnetic selection (Clinimacs Prodigy or equivalent). Assess viability (Trypan Blue) and purity (flow cytometry for CD34+).
- Ex Vivo CRISPR-Cas9 Editing: Electroporate the CD34+ cell suspension with SpCas9 ribonucleoprotein (RNP) complex targeting the BCL11A erythroid enhancer (+58 BCL11A binding site). Use optimized buffer systems and electrical parameters. Include a non-edited control aliquot.
- Product Formulation and Release Testing: Culture edited cells briefly in cytokine-supplemented media. Formulate final drug product in cryopreservation medium. Perform release assays: a) Viability (flow cytometry), b) Potency (indel frequency at target site via NGS), c) Vector Copy Number (qPCR for residual plasmid), d) Sterility (bacterial/fungal culture, mycoplasma), e) Purity (CD34+%, residual RNP components).
- Functional Validation (In Vitro): Differentiate a sample of the product towards erythropoiesis in a 3-phase erythroid culture system. At day 18-21, assess: a) Fetal Hemoglobin (HbF) Expression: Flow cytometry for F-cells and HPLC for HbF%. b) BCL11A Expression: qRT-PCR.
Protocol 2: Comparative Engraftment & Clonal Tracking in Murine Models
This protocol compares the dynamics of autologous edited vs. allogeneic grafts.
- Model Establishment: Use immunodeficient NSG mice or humanized sickle mouse models.
- Cell Preparation:
- exa-cel arm: Transplant human CD34+ cells edited per Protocol 1 after sublethal irradiation.
- Allo-HSCT arm: Transplant HLA-mismatched human CD34+ cells (simulating unrelated donor) into irradiated recipients.
- Control arm: Transplant non-edited autologous CD34+ cells.
- Engraftment Monitoring: Collect peripheral blood via retro-orbital bleeding at weeks 4, 8, 12, and 16. Use flow cytometry to quantify a) Human CD45+ Chimerism, b) Lineage distribution (CD19+, CD33+, CD235a+).
- Clonal Dynamics Analysis: At endpoint (week 16), harvest bone marrow. Isolate human CD45+ cells. Perform single-cell DNA sequencing or tracking of integration sites (for edited cells) to assess clonal diversity and presence of dominant clones. Compare polyclonality between exa-cel and allo-HSCT arms.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for BCL11A Editing & HSCT Comparative Research
| Item | Function in Research | Example/Supplier |
|---|---|---|
| Clinical-grade CD34+ Selection Kit | Isolation of target HSPCs from apheresis product with high purity for manufacturing or research-scale editing. | CliniMACS CD34 Reagent (Miltenyi Biotec) |
| GMP-grade CRISPR-Cas9 RNP | cGMP-manufactured Cas9 protein and target-specific sgRNA for clinical editing; ensures consistency and reduces regulatory risk. | Synthego, Thermo Fisher Precision GMP CRISPR |
| Myeloablative Conditioning Agent (Busulfan) | In vivo agent to create marrow niche for engraftment in both exa-cel and allo-HSCT preclinical models. | Busulfex (clinical analog for murine studies) |
| Erythroid Differentiation Media Kit | Standardized cytokine cocktails (SCF, EPO, IL-3, etc.) for in vitro differentiation of HSPCs to assess HbF upregulation. | StemSpan Erythroid Expansion Kit (Stemcell Tech) |
| NGS Target Amplicon Kit | High-sensitivity quantitation of on-target editing efficiency and identification of indel spectra in the BCL11A enhancer region. | Illumina MiSeq, IDT xGen Amplicon Panels |
| Clonal Tracking Library Prep Kit | For preparing libraries from integration site analysis (LAM-PCR, DPS-PCR) or single-cell DNA barcoding to monitor clonal dynamics. | Nextera DNA Library Prep Kit (Illumina) |
| Anti-Human HbF Antibody (PE conjugate) | Flow cytometric detection of F-cells (HbF+ erythroid cells) in differentiated cultures or patient samples post-treatment. | BD Biosciences Anti-Hemoglobin F (clone 2D12) |
| Immunosuppressants (for in vivo models) | Mimic post-allo-HSCT regimen in humanized mouse models (e.g., tacrolimus, sirolimus) to study GvHD. | Prograf (tacrolimus), Rapamune (sirolimus) |
Visualizations
Title: Therapeutic Pathways: exa-cel vs Allo-HSCT
Title: Molecular Mechanism of BCL11A Enhancer Editing by exa-cel
Benchmarking Against Other Genome Editing Strategies (e.g., Base Editing, Prime Editing)
Application Notes
Within the context of developing and validating exagamglogene autotemcel (exa-cel), a CRISPR-Cas9-based cell therapy for sickle cell disease and β-thalassemia targeting the BCL11A erythroid-specific enhancer, benchmarking against newer editing technologies is critical. These comparisons inform strategic decisions for next-generation therapies regarding efficiency, precision, and safety.
Key Benchmarking Parameters:
- Editing Efficiency: The percentage of alleles with the intended modification at the target locus.
- Product Purity: The proportion of desired edits (e.g., enhancer disruption) versus unintended byproducts (indels, other mutations).
- Genomic Safety: Off-target editing rates and the generation of chromosomal abnormalities (e.g., large deletions, translocations).
- Functional Outcome: The resulting levels of fetal hemoglobin (HbF) reactivation in edited hematopoietic stem and progenitor cells (HSPCs).
Table 1: Benchmarking of Genome Editing Strategies at the BCL11A Enhancer in HSPCs
| Editing Strategy | Target | Typical Editing Efficiency (%) | Product Purity (Desired Edit/Total Edits) | Primary Byproducts | Reported Off-target Risk (vs. SpCas9) | Key Advantage for BCL11A Targeting |
|---|---|---|---|---|---|---|
| CRISPR-Cas9 NHEJ (exa-cel) | BCL11A enhancer | 70-90% (indels) | ~80-90% | Small indels, large deletions | Baseline (1x) | Proven clinical efficacy; high efficiency. |
| CRISPR-Cas9 HDR | BCL11A enhancer | 10-30% (precise edit) | ~60-80% | Undesired indels, allele dropout | 1x | Enables precise nucleotide changes. |
| Adenine Base Editor (ABE) | Specific enhancer base(s) | 40-70% (conversion) | >95% | Rare non-A-to-G edits, bystander edits | Lower (0.1-0.5x) | High purity, no DSB, can disrupt transcription factor binding sites precisely. |
| Cytosine Base Editor (CBE) | Specific enhancer base(s) | 30-60% (conversion) | >90% | C-to-T bystander edits, C-to-G/A | Variable | Can create stop codons or disrupt motifs without DSBs. |
| Prime Editor (PE) | BCL11A enhancer | 20-50% (precise edit) | >99% | Small indels, incomplete edits | Lowest (<0.1x) | Ultimate versatility for any precise change; minimal byproducts. |
Data compiled from recent preclinical studies (2022-2024). Efficiency and purity ranges depend on delivery method, gRNA design, and cell type.
Table 2: Functional Outcomes of Different Editing Strategies on HbF Reactivation
| Strategy | HbF% in Edited Erythroid Progeny | Enucleation Efficiency | Proliferation/Engraftment Impact | Therapeutic Relevance |
|---|---|---|---|---|
| exa-cel (NHEJ) | 25-40% | Normal | Preserved | Clinically validated. |
| ABE (e.g., motif disruption) | 20-35% | Normal | Preserved | Potential safety advantage (no DSB). |
| PE (e.g., precise enhancer knockout) | 15-30% | Normal | Preserved under optimal conditions | High precision for complex edits. |
Experimental Protocols
Protocol 1: Benchmarking Editing Efficiency and Purity by Next-Generation Sequencing (NGS)
Objective: To quantitatively compare the editing outcomes (efficiency, spectrum) of Cas9 NHEJ, Base Editing, and Prime Editing at the BCL11A enhancer locus in primary human CD34+ HSPCs.
Materials (Research Reagent Solutions):
- Primary Human CD34+ HSPCs: Mobilized peripheral blood or cord blood-derived.
- Editing Reagents: In vitro transcribed or synthetic gRNA; SpCas9 protein (for NHEJ); ABE8e or PE2 mRNA; proprietary delivery reagents (e.g., electroporation kits).
- Cell Culture Media: SFEM II supplemented with cytokines (SCF, TPO, FLT3L).
- Lysis Buffer: QuickExtract DNA Extraction Solution.
- PCR Reagents: High-fidelity polymerase, primers flanking the BCL11A enhancer target site.
- NGS Library Prep Kit: For amplicon sequencing (e.g., Illumina MiSeq).
Procedure:
- Cell Preparation: Thaw and pre-stimulate CD34+ cells for 48 hours.
- Electroporation: Using a certified electroporator, deliver ribonucleoprotein (RNP) complexes for Cas9 or mRNA for Base/Prime Editors alongside their respective guide RNAs. Include a non-edited control.
- Recovery & Expansion: Culture cells for 5-7 days post-editing. Harvest an aliquot for genomic DNA extraction using QuickExtract.
- Target Site Amplification: Perform PCR with barcoded primers to generate amplicons spanning the edit window.
- NGS Library Preparation & Sequencing: Pool purified amplicons and prepare library per kit instructions. Sequence on a MiSeq system (2x300 bp).
- Data Analysis: Use specialized software (CRISPResso2, BE-Analyzer, PE-Analyzer) to quantify: a) Indel frequency (NHEJ), b) Base conversion efficiency (BE), c) Precise edit rate (PE), and d) the spectrum of all sequencing reads.
Protocol 2: Functional Benchmarking via Erythroid Differentiation and HbF Analysis
Objective: To assess the functional consequence of different editing strategies on HbF reactivation.
Procedure:
- Edit CD34+ HSPCs as in Protocol 1.
- Erythroid Differentiation: At day 7 post-editing, initiate a 3-phase erythroid differentiation culture system using specific cytokine cocktails (EPO, IL-3, stem cell factor).
- Harvest Cells: Collect cells at late erythroid stage (day 18-21).
- Flow Cytometry for HbF: Fix and permeabilize cells. Stain intracellularly with antibodies against HbF and adult hemoglobin (HbA). Analyze by flow cytometry to determine the percentage of HbF-positive cells and HbF content per cell.
- HPLC Analysis: Prepare lysates and run on a HPLC system with a cation-exchange column to separate and quantify HbF tetramers relative to total hemoglobin.
Visualization
Diagram 1: Logic of Editing Strategies for BCL11A
Diagram 2: Benchmarking Experimental Workflow
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for BCL11A Enhancer Editing Benchmarking
| Reagent/Material | Function | Example/Catalog Consideration |
|---|---|---|
| CD34+ HSPCs | Primary human cell model for evaluating therapeutic editing. | Mobilized peripheral blood, cord blood; must ensure high viability and stemness. |
| CRISPR-Cas9 RNP | Gold standard for NHEJ-mediated disruption. | Recombinant SpCas9 protein + synthetic sgRNA targeting the BCL11A enhancer. |
| Base Editor mRNA | Enables direct, DSB-free base conversion. | In vitro transcribed mRNA for ABE8e (for A-to-G) with appropriate sgRNA. |
| Prime Editor mRNA | Enables precise, versatile edits without DSBs. | In vitro transcribed mRNA for PE2 with a pegRNA encoding the desired edit. |
| Electroporation System | Critical for efficient delivery of editors into HSPCs. | Lonza 4D-Nucleofector with optimized P3 Primary Cell kit. |
| NGS Amplicon-Seq Kit | For quantitative, deep sequencing of on-target edits. | Illumina MiSeq Reagent Kit v3 (600-cycle) with custom index primers. |
| Erythroid Differentiation Media | To generate erythroid progeny for functional HbF assessment. | Custom multi-phase cytokine cocktail (SCF, EPO, IL-3, etc.) in serum-free base. |
| Anti-HbF Antibody | To measure functional protein output by flow cytometry. | Fluorescently conjugated monoclonal antibody (e.g., FITC anti-HbF). |
Conclusion
The BCL11A enhancer editing protocol for exagamglogene autotemcel represents a paradigm shift in the treatment of hemoglobinopathies, validating a highly precise CRISPR-Cas9 strategy to reactivate fetal hemoglobin. This guide has detailed its foundational science, rigorous manufacturing methodology, solutions for critical optimization hurdles, and compelling clinical validation. Key takeaways include the achievement of durable clinical benefits with a manageable safety profile, though long-term monitoring remains essential. The success of exa-cel paves the way for next-generation refinements in delivery, editing precision, and accessibility. Future directions include exploring in vivo delivery platforms, applying similar enhancer-editing logic to other disorders, and streamlining manufacturing to broaden global access, cementing targeted enhancer editing as a cornerstone of future genomic medicine.