AAV Vectors for Base Editing: A Comprehensive Guide for Therapeutic Gene Editing Research
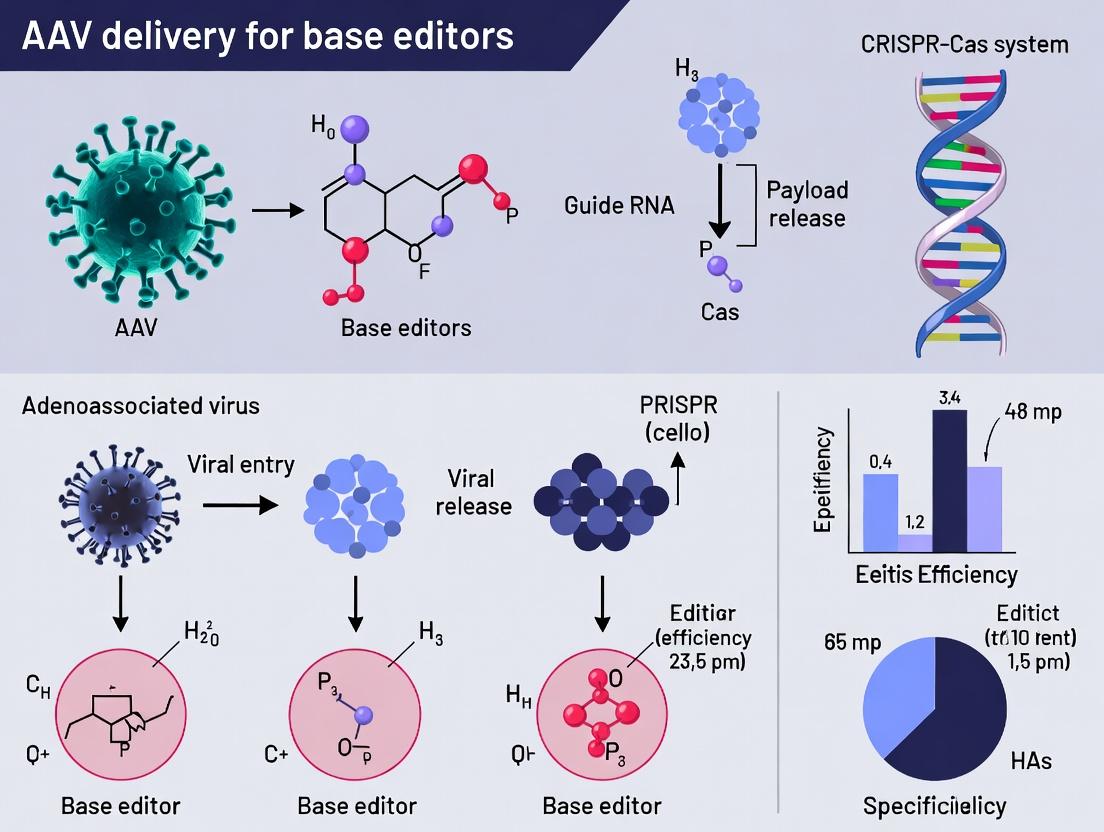
This article provides a detailed guide for researchers and drug developers on utilizing Adeno-Associated Virus (AAV) vectors to deliver base editors for precise gene correction.
AAV Vectors for Base Editing: A Comprehensive Guide for Therapeutic Gene Editing Research
Abstract
This article provides a detailed guide for researchers and drug developers on utilizing Adeno-Associated Virus (AAV) vectors to deliver base editors for precise gene correction. It covers foundational principles of AAV biology and base editor architecture, explores current methodologies for vector design and in vivo delivery, addresses critical troubleshooting and optimization challenges including immunogenicity and off-target effects, and validates approaches through comparative analysis of recent preclinical and clinical studies. The synthesis offers a strategic roadmap for advancing AAV-base editor therapies toward clinical application.
Understanding the Core Principles: AAV Biology Meets Base Editor Architecture
Adeno-associated virus (AAV) vectors are a cornerstone of modern gene therapy and functional genomics research. Within the context of developing base editor delivery systems, understanding the AAV toolkit—specifically serotype selection for optimal tropism, and the constraints of packaging capacity—is critical for designing effective in vivo and ex vivo experiments. This document provides application notes and detailed protocols for leveraging AAV in base editing research.
AAV Serotypes & Tissue Tropism
AAV serotypes exhibit distinct tissue tropism due to variations in their capsid proteins, which interact with different cell surface receptors. Selecting the appropriate serotype is paramount for targeting specific tissues in base editing applications.
Table 1: Common AAV Serotypes and Their Primary Tropism
| Serotype | Primary Tropism in Rodents/Models | Common Applications in Gene Editing |
|---|---|---|
| AAV1 | Skeletal muscle, heart | Muscle-targeted base editing |
| AAV2 | Liver, CNS neurons, retinal cells | Early proof-of-concept studies |
| AAV5 | CNS neurons, photoreceptors, lung | CNS and pulmonary base editing |
| AAV6 | Heart, lung, skeletal muscle | Cardiomyocyte and airway editing |
| AAV8 | Liver, pancreas, retina | Hepatic-focused base editing |
| AAV9 | Broad systemic, heart, CNS, liver | Whole-body/base editor delivery |
| AAV-DJ | Broad, enhanced in vitro transduction | Screening and in vitro work |
| AAV-PHP.eB / .S | Enhanced CNS tropism (mice) | CNS-targeted base editing in mice |
| AAV-LK03 / AAV3B | Enhanced human hepatocyte tropism | Humanized liver model editing |
| AAVrh.10 | CNS, retina, lung | Alternative CNS delivery |
Packaging Capacity Constraints
The ~4.7 kb packaging limit of AAV is a significant constraint for delivering base editing systems, which typically exceed this size.
Table 2: Packaging Strategies for Large Base Editor Constructs
| Strategy | Maximum Effective Payload | Mechanism | Advantages | Disadvantages |
|---|---|---|---|---|
| Single Vector (Full) | ~4.7 kb | Deliver BE as a single expression cassette | Simple production, consistent stoichiometry | Limited to compact BEs (e.g., ABE8e, some CGBEs) |
| Dual Vector (Trans-splicing) | ~9.4 kb | Split BE cDNA between two AAVs, reconstitute via ITR-mediated recombination | Delivers large BEs or BEs with regulatory elements | Lower efficiency, risk of incomplete reconstitution |
| Dual Vector (Overlapping) | ~6.0 kb | Two AAVs with overlapping homology regions, reconstitute via homologous recombination | Can be more efficient than trans-splicing | Complex vector design, potential for truncated proteins |
| Miniaturized Editors | Varies | Use truncated deaminases (e.g., evoAPOBEC1, Anc689) and compact Cas9 variants (e.g., saCas9, cjCas9) | Fits in single AAV with room for promoters/regulatory elements | May have reduced activity or altered PAM requirements |
Application Notes for Base Editing Research
- Tropism Validation: Always validate serotype tropism in your specific animal model and target tissue. Cross-species differences are common.
- Promoter Selection: Use tissue-specific or synthetic promoters (e.g., synPmin, EFS) within the packaging limit to restrict/enhance expression.
- Dosing Considerations: For dual-vector systems, a 1:1 molar ratio of the two vectors is standard, but empirical titration is recommended.
- Off-Target & Safety: Include appropriate controls (e.g., nuclease-dead base editor) and plan for analyses of off-target editing and potential immunogenicity.
Detailed Protocols
Protocol 1: Production of AAV Vectors for Base Editors
Objective: Generate high-titer, high-purity AAV vectors for in vivo base editing experiments.
Research Reagent Solutions Toolkit:
| Item | Function |
|---|---|
| pAAV Transfer Plasmid | Contains ITRs flanking the base editor expression cassette. |
| pHelper Plasmid | Provides adenoviral helper functions (E4, E2a, VA RNA). |
| Rep/Cap Plasmid | Supplies AAV replication (Rep) and desired serotype capsid (Cap) proteins. |
| HEK293T/AAV293 Cells | Production cell line expressing adenoviral E1 genes. |
| Polyethylenimine (PEI) Max | Transfection reagent for co-delivery of three plasmids. |
| Benzonase Nuclease | Degrades unpackaged nucleic acids during purification. |
| Iodixanol Gradient Media | For ultracentrifugation-based purification of AAV particles. |
| AAVpro Purification Kit | Column-based purification system for rapid, high-purity AAV prep. |
| qPCR Kit with ITR Primers | For accurate quantification of viral genome titer (vg/mL). |
| Anti-AAV Capsid Antibody | For ELISA-based quantification of total viral particle titer. |
Methodology:
- Day 0: Seed Cells. Seed HEK293T cells in 15-cm dishes at ~70% confluency in DMEM + 10% FBS.
- Day 1: Transfection. For one dish, prepare DNA mix: 1.5 µg pHelper, 1.0 µg Rep/Cap, 2.0 µg pAAV-BE plasmid in 1 mL serum-free DMEM. In a separate tube, dilute 18 µL PEI Max (1 mg/mL) in 1 mL serum-free DMEM. Combine, vortex, incubate 15 min at RT. Add dropwise to cells.
- Day 2: Media Change. Replace transfection media with fresh complete media.
- Day 5: Harvest & Purify. a. Collect cells and media. Pellet cells (500 x g, 5 min). b. Resuspend pellet in lysis buffer (150 mM NaCl, 50 mM Tris, pH 8.5). Freeze-thaw 3x. c. Treat lysate with Benzonase (50 U/mL, 37°C, 30 min) to digest residual DNA/RNA. d. Clarify lysate by centrifugation (3,000 x g, 15 min). e. Purify supernatant via iodixanol step gradient ultracentrifugation (15%, 25%, 40%, 60% layers) at 350,000 x g for 2 hours. f. Collect the opaque band at the 40-60% interface. Desalt/concentrate using a 100kDa MWCO centrifugal filter.
- Titering: Quantify viral genome titer by qPCR using primers/probe against the ITR region. Aliquot and store at -80°C.
Protocol 2:In VivoDelivery & Analysis of AAV-Base Editors
Objective: Administer AAV-base editor and assess editing efficiency in target tissue.
Methodology:
- Animal Preparation: Anesthetize mice according to approved IACUC protocol.
- Administration:
- Systemic (e.g., liver): Inject appropriate dose (e.g., 1e11 - 5e11 vg/mouse) via retro-orbital or tail vein in 100 µL sterile PBS.
- Local (e.g., CNS): Perform stereotactic injection into the target brain region.
- Tissue Harvest: Euthanize animals at prescribed timepoint (e.g., 2-4 weeks post-injection). Collect and snap-freeze target tissue.
- Genomic DNA Extraction: Use a commercial tissue DNA extraction kit.
- Editing Analysis: a. PCR Amplification: Amplify the target genomic locus from extracted DNA. b. Next-Generation Sequencing (NGS): Prepare amplicon NGS libraries and sequence on an Illumina platform. c. Data Analysis: Use computational tools (e.g., CRISPResso2, BE-Analyzer) to quantify base conversion efficiency and indel rates.
Visualization Diagrams
Title: AAV Cellular Entry and Transduction Pathway
Title: Decision Workflow for AAV Base Editor Packaging
Application Notes: AAV Delivery of Base Editors for Therapeutic Research
Base editing enables precise, programmable conversion of single DNA bases without requiring double-stranded DNA breaks (DSBs) or donor templates. This technology is particularly promising for correcting point mutations underlying genetic diseases. Adeno-associated virus (AAV) serves as the dominant delivery vehicle for in vivo base editor therapies due to its low immunogenicity, tropism flexibility, and established clinical safety profile. However, the packaging capacity of AAV (~4.7 kb) presents a significant constraint for delivering base editors, which are large fusion proteins.
Key Constraint & Engineering Solution: A canonical cytosine base editor (CBE), such as BE4max, comprises a Cas9 nickase (nCas9), a cytidine deaminase (e.g., APOBEC1), and an uracil glycosylase inhibitor (UGI). This often exceeds AAV's cargo limit. Strategies to overcome this include:
- Dual-AAV Systems: Splitting the base editor into two AAV vectors, one encoding the nCas9 fusion and the other encoding the deaminase/accessory proteins, reconstituted via intein splicing or trans-splicing.
- Miniaturization: Using smaller Cas9 orthologs (e.g., SaCas9, Nme2Cas9) and compact deaminases (e.g., SECURE-engineered APOBEC1, Anc689) to fit within a single AAV.
Recent Efficacy Data (2023-2024): The following table summarizes recent in vivo studies using AAV-delivered base editors:
Table 1: Recent In Vivo AAV-Base Editor Studies
| Target Disease (Model) | Base Editor Type | AAV Strategy | Delivery Route | Avg. Editing Efficiency (Range) | Key Outcome | Reference (Preprint/Journal) |
|---|---|---|---|---|---|---|
| Progeria (LmnaG609G/+ mouse) | ABE8e (Nme2Cas9) | Single AAV (Nme2ABE8e) | Systemic (P0) | 22% (Liver) | Extended lifespan from 7 to 17 months. | Nature, 2023 |
| Hypercholesterolemia (Pcsk9 mouse) | miniCBE (SaCas9-APOBEC1) | Single AAV | Systemic | 63% (Liver) | Durable >50% reduction in PCSK9 and LDL cholesterol. | Nat. Commun., 2023 |
| Retinal degeneration (Rpe65 mouse) | CBE (SpCas9-nCas9) | Dual AAV (trans-splicing) | Subretinal | 44% (RPE) | Restored RPE65 function and visual acuity. | Sci. Adv., 2024 |
| Tyrosinemia (Fah mouse) | CBE (SpG-APOBEC1) | Dual AAV (intein) | Hydrodynamic Injection | 31% (Liver) | Selected for corrected hepatocytes, rescued survival. | Cell, 2023 |
Critical Considerations for AAV Delivery:
- Immunogenicity: Pre-existing antibodies against AAV capsids or the bacterial-derived Cas9 protein can limit transduction and efficacy.
- Off-Target Editing: Includes DNA off-targets (deaminase activity at non-target loci) and RNA off-targets (promiscuous deaminase activity on cellular transcripts). Newer engineered deaminases (e.g., SECURE-ABEs, eA3A-CBE) show markedly reduced RNA off-targets.
- Bystander Editing: Within the activity window (typically ~5 nucleotides), non-target bases may be edited. Careful sgRNA design is crucial to position the disease-relevant base optimally.
- Long-Term Expression: AAV can lead to sustained base editor expression, increasing off-target risks. Self-inactivating vectors or delivery of editor as transient mRNA/protein are under investigation.
Detailed Protocols
Protocol 1: Evaluating AAV-Base Editor EfficiencyIn VitroPrior toIn VivoUse
Aim: To quantify on-target base editing efficiency and byproduct indels in cultured cells using a dual-AAV8 system delivering a split BE4max editor.
Materials (Research Reagent Solutions):
| Reagent/Material | Function/Explanation |
|---|---|
| HEK293T cells (ATCC CRL-3216) | Standard cell line for high transfection efficiency and AAV production. |
| Dual-AAV8-BE4max system (VectorBuilder) | One AAV encodes nCas9-UGI, the other encodes APOBEC1; split via intein. |
| Target-specific sgRNA plasmid | Guides base editor to genomic locus of interest. |
| QuickExtract DNA Solution (Lucigen) | Rapid, simple preparation of PCR-ready genomic DNA. |
| Phire Animal Tissue Direct PCR Kit (Thermo) | For direct PCR amplification from genomic DNA for sequencing. |
| Sanger Sequencing & EditR (or ICE) Analysis | For quantification of base conversion frequencies from sequencing traces. |
| T7 Endonuclease I (NEB) | Detects indel formation resulting from residual DSB activity. |
Methodology:
- Cell Seeding: Seed HEK293T cells in a 24-well plate at 1.5 x 10^5 cells/well.
- Co-transduction: 24 hours later, co-transduce cells with both AAV8-BE4max vectors (MOI of 1e5 vg/cell each) and the sgRNA plasmid (250 ng) using polyethylenimine (PEI).
- Harvest: 72 hours post-transduction, aspirate media, wash with PBS, and add 100 µL QuickExtract to each well. Incubate at 65°C for 15 min, 98°C for 10 min.
- PCR Amplification: Amplify the target genomic locus using 2 µL of extract with the Phire PCR kit. Purify the amplicon.
- Efficiency Analysis: Submit purified PCR product for Sanger sequencing. Analyze the chromatogram using the EditR web tool (moriaritylab.shinyapps.io/EditR/) to calculate the percentage of C-to-T (or A-to-G for ABE) conversion.
- Indel Analysis: Using the same purified PCR product, perform a T7 Endonuclease I assay per manufacturer's instructions to detect and quantify any indel formation, which indicates DSB formation and NHEJ.
Protocol 2: AssessingIn VivoBase Editing in Mouse Liver via AAV8/9
Aim: To measure base editing outcomes following systemic delivery of a single-AAV packaged mini-base editor targeting Pcsk9.
Materials (Research Reagent Solutions):
| Reagent/Material | Function/Explanation |
|---|---|
| C57BL/6 mice (6-8 weeks) | Standard inbred mouse strain for preclinical liver studies. |
| AAV9-miniCBE (targeting mouse Pcsk9) | Single AAV encoding SaCas9-APOBEC1-UGI under a liver-specific promoter. |
| 1x PBS, pH 7.4 | Vehicle for AAV dilution and injection. |
| Isoflurane Anesthesia System | For humane restraint of mice during injection. |
| Insulin syringes (0.5 mL, 29G) | For precise intravenous tail vein injection. |
| DNeasy Blood & Tissue Kit (Qiagen) | High-quality genomic DNA extraction from liver tissue. |
| Illumina MiSeq Amplicon Sequencing | High-depth sequencing to quantify editing efficiency, bystander edits, and rare indels. |
| CRISPResso2 (Software) | Bioinformatics tool for analyzing next-generation sequencing data of edited amplicons. |
Methodology:
- AAV Preparation: Dilute AAV9-miniCBE in sterile PBS to a dose of 5e11 vector genomes (vg) in a total volume of 100 µL per mouse.
- Animal Injection: Anesthetize mouse with isoflurane. Warm the tail under a heat lamp to dilate the vein. Slowly inject 100 µL of AAV solution intravenously via the lateral tail vein.
- Tissue Collection: At 2-4 weeks post-injection, euthanize the mouse and perfuse the liver with cold PBS via the portal vein. Collect and snap-freeze liver lobes in liquid nitrogen.
- Genomic DNA Extraction: Homogenize ~25 mg of liver tissue and extract genomic DNA using the DNeasy kit. Elute in 100 µL nuclease-free water.
- Amplicon Sequencing Library Prep: Design primers flanking the target site (~250 bp amplicon). Perform a two-step PCR: (1) Amplify target from gDNA, (2) Add Illumina adapters and sample barcodes. Pool and purify libraries.
- Sequencing & Analysis: Sequence pooled libraries on an Illumina MiSeq (2x300 bp). Process reads using CRISPResso2 with the
--base_editorflag set to "CBE" and appropriate quantification windows. Output includes: primary base conversion percentage, bystander edit rates, and indel frequency.
Visualizations
Title: AAV Base Editor Delivery Strategies
Title: Base Editor Architecture & Function
Title: Base Editor Mechanism of Action
Why AAV for Base Editors? Rationale for In Vivo Delivery of Precision Gene Editors.
Adeno-associated virus (AAV) has emerged as the predominant vector for the in vivo delivery of base editors (BEs). This preference is rooted in AAV's favorable safety profile, its ability to transduce both dividing and non-dividing cells across numerous tissues, and the sustained transgene expression it often enables. Within the broader thesis of AAV delivery for BE research, this application note details the rationale, key experimental data, and protocols for deploying AAV-BE systems in vivo.
Rationale and Comparative Advantages
Table 1: Rationale for Using AAV to Deliver Base Editors In Vivo
| Criterion | AAV Advantages for BE Delivery | Key Implication for Base Editing |
|---|---|---|
| Safety | Non-pathogenic; low immunogenicity relative to other viral vectors. | Enables safer human therapeutic application and repeat dosing in some serotypes. |
| Tropism | Multiple natural and engineered serotypes target specific tissues (e.g., AAV9 for CNS/heart, AAV8 for liver). | Allows precise targeting of therapeutically relevant cell types in vivo. |
| Payload Capacity | ~4.7 kb packaging limit. | Fits BE proteins (e.g., AncBE4max: ~5.2 kb) with compact promoters, but requires dual-vector or split-intein strategies for larger BEs or with additional regulatory elements. |
| Duration of Expression | Long-term episomal persistence in non-dividing cells; potential for genomic integration at low frequency. | Ideal for correcting genetic diseases in post-mitotic tissues, leading to durable editing. |
| Immunogenicity | Capsid and transgene can elicit humoral and cellular immune responses. | A significant consideration for clinical translation; may limit re-administration. |
Table 2: Quantitative Comparison of Viral Vectors for In Vivo Base Editing
| Vector | Max Payload | Integration Risk | Titer (vg/mL) | In Vivo Editing Efficiency (Typical Range) | Primary Limitation for BEs |
|---|---|---|---|---|---|
| AAV | ~4.7 kb | Very Low (episomal) | 1e13 - 1e14 | 5-60% (tissue-dependent) | Limited cargo capacity. |
| Lentivirus | ~8 kb | High (random) | 1e8 - 1e9 TU/mL | N/A (integrating) | Unsuitable for in vivo due to integration risk. |
| Adenovirus | ~8-36 kb | Low (episomal) | 1e10 - 1e12 IU/mL | High (transient) | High immunogenicity, transient expression. |
Key Experimental Protocols
Protocol 1: Production and Purification of AAV-Base Editor Vectors
Objective: Generate high-titer, research-grade AAV stocks encoding a base editor.
Materials (Research Reagent Solutions):
- pAAV-BE Expression Plasmid: Contains BE gene (e.g., ABE8e) under a tissue-specific promoter (e.g., liver-specific TBG).
- pAAV Rep2/Cap8 Plasmid: Provides AAV2 replication proteins and serotype 8 capsid for liver tropism.
- pAdHelper Plasmid: Supplies adenoviral helper functions (E4, E2a, VA RNA).
- PEI MAX 40K: Transfection reagent for HEK293T cells.
- HEK293T Cells: Adherent cell line for AAV production.
- Iodixanol Gradient Solution: For ultracentrifugation-based purification of AAV particles.
- AAVpro Titration Kit (Takara Bio): For quantifying viral genome titer via qPCR.
Procedure:
- Triple Transfection: Seed 15-cm plates with HEK293T cells. At 70-80% confluency, co-transfect using PEI MAX with pAAV-BE, pAAV-Rep2/Cap8, and pAdHelper at a 1:1:1 molar ratio.
- Harvest: 72 hours post-transfection, collect cells and media. Lyse cells via freeze-thaw cycles and benzonase treatment to degrade unpackaged DNA.
- Iodixanol Gradient Ultracentrifugation: Purify AAV particles on a discontinuous iodixanol gradient (15%, 25%, 40%, 60%) via ultracentrifugation (350,000 x g, 2 hours). Collect the 40% fraction containing purified AAV.
- Concentration & Buffer Exchange: Concentrate and exchange into PBS-MK buffer using a 100kDa MWCO centrifugal filter.
- Titration: Determine viral genome (vg) titer using qPCR against a standard curve (e.g., AAVpro Titration Kit). Aliquot and store at -80°C.
Protocol 2:In VivoDelivery and Assessment of AAV-Base Editors in Mouse Liver
Objective: Assess the efficiency and specificity of liver-targeted base editing.
Materials:
- AAV8-BE: Purified AAV8 vector expressing BE (e.g., targeting Pcsk9) under a TBG promoter. Dose: 1e11 - 5e11 vg per mouse via tail vein.
- C57BL/6 Mice: 6-8 week old.
- Guide RNA: Encoded within the AAV vector or co-delivered.
- Plasma Collection Tubes: For collecting blood to assess serum PCSK9/protein levels.
- Genomic DNA Extraction Kit: For isolating liver DNA.
- Next-Generation Sequencing (NGS) Library Prep Kit: For assessing on-target and off-target editing.
Procedure:
- Animal Injection: Administer AAV8-BE vector via tail vein injection into mice (n=5 per group).
- Monitoring & Sample Collection: At 2- and 4-weeks post-injection, collect blood for plasma analysis. At 4 weeks, euthanize animals and harvest liver lobes.
- Molecular Analysis:
- Genomic DNA Extraction: Isolve DNA from ~25 mg of liver tissue.
- On-target PCR: Amplify the genomic region surrounding the target site.
- NGS Library Preparation & Sequencing: Prepare amplicon libraries for deep sequencing (minimum 100,000x coverage).
- Data Analysis: Use computational pipelines (e.g., CRISPResso2) to quantify the percentage of C•G to T•A or A•T to G•C conversion and indel frequencies.
- Phenotypic Assessment: Measure serum PCSK9 levels via ELISA to confirm functional correction.
The Scientist's Toolkit
Table 3: Essential Reagents for AAV-BE In Vivo Research
| Reagent / Kit | Provider Examples | Function in Workflow |
|---|---|---|
| AAV Helper-Free System | Agilent, Cell Biolabs | Provides all plasmids needed for AAV production in a triple-transfection. |
| AAVpro Purification Kit | Takara Bio | All-in-one kit for purification via iodixanol gradient or affinity chromatography. |
| AAV Titration Kit (qPCR) | Takara Bio, Applied Biological Materials | Accurately determines the viral genome titer of purified stocks. |
| In Vivo-JetPEI | Polyplus-transfection | In vivo-grade transfection reagent for direct in vivo delivery of BE RNPs as a control. |
| Next-Generation Sequencing Kit | Illumina, IDT | For preparing amplicon-seq libraries to quantify base editing efficiency and byproducts. |
| CRISPResso2 | Open-source software | Critical computational tool for analyzing NGS data from base editing experiments. |
Visualizations
AAV-BE In Vivo Delivery Pathway
Dual AAV Strategy for Large BEs
Within the broader thesis on recombinant Adeno-Associated Virus (AAV) delivery for in vivo base editing, three paramount challenges constrain clinical translation: the inherent Packaging Size Constraint of AAV (~4.7 kb), pre-existing and therapy-induced Immunogenicity, and the trade-offs associated with Persistent Expression. This document provides detailed application notes and experimental protocols to navigate these challenges, enabling robust research and development.
Packaging Size Constraints: Strategies and Validation
The limited AAV cargo capacity is incompatible with standard SpCas9-based base editors (BE). The primary solution is the adoption of compact editors.
Table 1: Compact Base Editors and Their Characteristics
| Editor System | Approximate Size (bp) | Origin/Modification | Key Advantage | Reported Editing Efficiency (Range)* |
|---|---|---|---|---|
| BE4max | ~5300 | SpCas9 | Too large for AAV | N/A (Dual-AAV required) |
| ABE8e | ~5200 | TadA-8e variant | High activity | 50-80% (in vivo liver) |
| SaCas9-KKH BE | ~4400 | Staphylococcus aureus Cas9 | Fits in AAV with regulatory elements | 20-45% |
| Nme2Cas9 BE | ~3900 | Neisseria meningitidis Cas9 | Fits in AAV with ease, good fidelity | 15-40% |
| Cpfl- (AsCas12f) BE | ~3300 | Ultra-small Cas12f | Enables addition of large regulatory elements | 10-30% (proof-of-concept) |
| Tiny BE (GkI-BE) | ~3200 | Geobacillus kaustophilus Cas9 | Smallest validated editor | 5-25% |
*Efficiency is tissue and target dependent. Data compiled from recent preprints (2023-2024).
Protocol 2.1: Validating Packaging Efficiency via Droplet Digital PCR (ddPCR)
Objective: Quantify the proportion of fully packaged AAV genomes containing the entire editor expression cassette. Materials:
- Purified AAV vector (serotype relevant to your model, e.g., AAV9 for liver).
- DNase I (to remove unpackaged DNA).
- ddPCR Supermix for Probes (no dUTP).
- Two TaqMan probe sets:
- Flanking Probe Set: Targets a region at the 5' end of the ITR-flanked genome (e.g., promoter).
- Internal/Junction Probe Set: Targets a region at the 3' end or spanning a critical junction (e.g., editor-reporter junction).
- Droplet generator and reader. Procedure:
- DNase Treatment: Incubate 5e9 vg of AAV with 2 U DNase I at 37°C for 30 min. Heat-inactivate at 75°C for 10 min.
- Viral Lysis & DNA Release: Add Proteinase K (final 0.5 mg/mL) and SDS (final 0.5%) to the sample. Incubate at 56°C for 60 min, then 95°C for 10 min.
- ddPCR Setup: Prepare two separate reactions for each probe set. Use ~1e7 vg equivalent of lysed DNA per 20 µL reaction. Generate droplets.
- PCR Cycling: Standard two-step cycling (95°C for 10 min, then 40 cycles of 94°C for 30 s and 60°C for 60 s).
- Analysis: Calculate concentration (copies/µL) for each probe set from the positive droplet count. The Packaging Efficiency (%) = (Concentration of Internal Probe / Concentration of Flanking Probe) * 100. Values <100% indicate truncated genomes.
Diagram 1: Dual-AAV vs Single-AAV Strategies
Diagram Title: Dual vs Single AAV Packaging Strategies
Immunogenicity: Assessment and Mitigation
Immunogenicity involves both cellular (T-cell) and humoral (neutralizing antibody, NAb) responses against the AAV capsid and the transgene product.
Table 2: Immunogenicity Assessment Methods
| Assay Type | Target | Sample Type | Readout | Information Gained |
|---|---|---|---|---|
| ELISpot | Capsid/Editor-specific T-cells | PBMCs or Splenocytes | IFN-γ spots | Frequency of reactive CD4+/CD8+ T-cells. |
| Humoral (NAb) Assay | Anti-AAV NAbs | Serum | Luciferase Inhibition | % neutralization; titer (critical for patient screening). |
| Intracellular Cytokine Staining (ICS) | Capsid/Editor-specific T-cells | PBMCs/Splenocytes | Flow Cytometry (IFN-γ, TNF-α) | Phenotype and frequency of reactive T-cells. |
| Anti-drug Antibodies (ADA) ELISA | Anti-base editor antibodies | Serum | Absorbance (450 nm) | Humoral response against the transgene product. |
Protocol 3.1:In VitroNeutralizing Antibody (NAb) Assay
Objective: Determine the neutralizing capacity of serum antibodies against a specific AAV serotype. Materials:
- HEK293T cells (70-80% confluent in 96-well plate).
- AAV-Luciferase reporter vector (same serotype as therapy, e.g., AAV9-Luc).
- Test serum (heat-inactivated at 56°C for 30 min).
- Control (NAb-negative) serum or PBS.
- Luciferase assay kit.
- Cell culture medium. Procedure:
- Serum Dilution: Prepare 4-fold serial dilutions of test serum in medium (e.g., 1:10 to 1:2560) in a separate 96-well plate.
- Virus-Serum Incubation: Add a fixed dose of AAV-Luc (e.g., 1e9 vg/well) to each serum dilution. Mix and incubate at 37°C for 1 hr.
- Infection: Transfer 50 µL of each mixture onto HEK293T cells (in triplicate). Include virus-only (no serum) and cell-only controls. Incubate for 48-72 hrs.
- Luciferase Measurement: Lyse cells and quantify luminescence per manufacturer's protocol.
- Analysis: Calculate % Neutralization = [1 - (RLUtest serum / RLUvirus-only control)] * 100. The NAb titer is often defined as the serum dilution that inhibits 50% of luciferase signal (ID50).
Diagram 2: Immunogenicity Pathways Post-AAV Delivery
Diagram Title: AAV-Induced Immune Pathways
Persistent Expression: Balancing Efficacy and Safety
Persistent editor expression increases the risk of off-target editing and immune recognition, yet is often required for high editing levels in slow-dividing tissues.
Protocol 4.1: Quantifying Editor Persistence via qPCR and Biodistribution
Objective: Track the kinetics of vector genome and editor mRNA persistence in target and off-target tissues. Materials:
- Tissues of interest (e.g., liver, heart, muscle, dorsal root ganglia, gonads).
- RNA/DNA co-extraction kit.
- cDNA synthesis kit.
- qPCR reagents (SYBR Green).
- Primers specific for:
- Vector Genome (DNA): Target a sequence within the transgene (avoiding regions of genomic homology).
- Editor mRNA (cDNA): Span an intron (if using an intron-containing expression cassette) to distinguish from genomic DNA.
- Reference Gene (DNA & cDNA): e.g., Rpp30 for mouse genomic DNA, Gapdh for mRNA. Procedure:
- Sample Collection: At multiple timepoints (e.g., 1wk, 4wks, 12wks, 24wks) post-AAV administration, harvest and snap-freeze tissues.
- Nucleic Acid Extraction: Co-purify genomic DNA and total RNA from the same tissue homogenate.
- cDNA Synthesis: Treat RNA with DNase I, then synthesize cDNA from equal RNA inputs.
- qPCR Quantification:
- For DNA: Dilute samples and run qPCR for vector genome and reference gene. Use a standard curve from a plasmid of known concentration to calculate vg/dg.
- For cDNA: Run qPCR for editor transcript and reference gene. Calculate relative expression (2^-ΔΔCt) or absolute copies via standard curve.
- Analysis: Plot vg/dg and relative mRNA expression over time. Compare persistence across tissues (biodistribution) and between different promoters (e.g., liver-specific vs. ubiquitous).
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function/Application in AAV-BE Research | Example/Vendor (Illustrative) |
|---|---|---|
| pAAV Vectors | Backbone plasmids for AAV production. Contain ITRs for packaging. | pAAV-ITR (Addgene #107790). |
| Compact Editor Plasmids | Expression constructs for SaCas9-BE, Nme2Cas9-BE, etc. | pCMV-SaCas9-KKH-ABE (Addgene #138499). |
| AAV Serotype Helper Kits | Provide rep/cap and adenoviral helper functions for specific serotypes (1-9, DJ, etc.). | AAVpro Helper Free System (Takara). |
| Pricing/Quantitation Standards | Linearized DNA standards for ddPCR/qPCR to absolutely quantify vg titer and biodistribution. | AAV9 Titration Standard (ATCC). |
| Neutralizing Antibody Assay Kits | Pre-packaged kits for standardized NAb detection against specific AAV serotypes. | AAV9 Neutralizing Antibody Assay Kit (Promega). |
| ELISpot Kits | For detecting IFN-γ secretion from T-cells responsive to capsid or editor peptides. | Mouse IFN-γ ELISpot PLUS (Mabtech). |
| Next-Gen Sequencing Library Prep Kits | For comprehensive off-target analysis (GUIDE-seq, CIRCLE-seq, or targeted amplicon sequencing). | Illumina DNA Prep. |
| Cell Lines for Tropism | In vitro models for testing AAV entry (e.g., HepG2 for liver, iPSC-derived neurons). | Various from ATCC, iXCells. |
Diagram 3: Trade-offs in Persistent Expression
Diagram Title: Pros and Cons of Persistent Expression
Designing and Delivering AAV-Base Editor Constructs: From Bench to Preclinical Models
Adeno-associated virus (AAV) vectors are a primary delivery vehicle for in vivo gene editing, including base editors. However, the ~4.7 kb packaging limit of AAV constrains delivery of larger constructs. This is a critical challenge in base editor delivery, as SpCas9-derived base editors often exceed this limit when combined with regulatory elements. This application note, framed within a thesis on AAV delivery for base editors, details and compares three primary strategies to overcome this limitation: single AAV systems (using truncated/minimized components), dual AAV systems (using split-intein or overlapping strategies), and trans-splicing AAVs. The choice of strategy significantly impacts editing efficiency, tissue tropism, immunogenicity, and translational feasibility.
Quantitative Comparison of Strategies
Table 1: Comparative Analysis of AAV Strategies for Large Payload Delivery
| Parameter | Single AAV (Minimized) | Dual AAV (Split-Intein) | Dual AAV (Overlapping) | Trans-Splicing AAV |
|---|---|---|---|---|
| Max Theoretical Payload | ~4.7 kb | ~9.4 kb (2 vectors) | ~9.4 kb (2 vectors) | >9.4 kb (2+ vectors) |
| Typical In Vivo Efficiency | Low to Moderate (Varies by tissue) | Moderate to High | Low to Moderate | Low (Dependent on concatemerization) |
| Key Advantage | Simplest production, predictable stoichiometry | High-fidelity reconstruction of full protein | No requirement for protein splicing | Can deliver very large genes |
| Primary Limitation | Severely limited payload size | Lower effective titer, intein splicing inefficiency | Homology-dependent low-efficiency recombination | Extremely low efficiency, complex vector design |
| Immunogenicity Concern | Standard AAV risk | Potential for intein immunogenicity | Standard AAV risk | Standard AAV risk |
| Common Use Case | Compact editors (e.g., saCas9-BE) | Standard SpCas9-BEs, dual-vector prime editors | Proof-of-concept studies | Delivery of genes >6 kb |
Table 2: Published Efficiencies of Base Editor Delivery via Dual AAV Systems (Recent Examples)
| Study (Year) | Target Tissue | Editor Delivered | Strategy | Reported Efficiency Range | Key Metric |
|---|---|---|---|---|---|
| Levy et al. (2020) | Mouse Liver | BE4max | Dual AAV (Split Intein) | 58% mean editing | % target base conversion |
| Villiger et al. (2021) | Mouse Liver | ABE8e | Dual AAV (Overlap) | Up to 42% | Indel-free correction |
| Zhang et al. (2022) | Mouse Brain | CBE | Dual AAV (Split Intein) | 351.8% (vs single AAV) | Fold-increase over single AAV |
| Richter et al. (2023) | NHP Liver | ABE | Single & Dual AAV | Dual: 25-47%, Single: 57%* | % editing (Single used compact editor) |
*This highlights that a well-optimized single AAV with a compact editor can outperform a dual system.
Protocols
Protocol 3.1: Production and Titration of Dual AAV (Split-Intein) Vectors
Objective: To produce two AAV vectors, each carrying one half of a split-intein-fused base editor, and determine their functional titer.
Materials: See "The Scientist's Toolkit" (Section 5).
Method:
- Vector Design: Split the base editor (e.g., BE4max) at a permissive site (e.g., SpCas9 residue 573/574). Fuse the N- and C-terminal fragments to split intein segments (e.g., Npu DnaE). Clone each fragment into separate AAV cis-plasmids containing inverted terminal repeats (ITRs), a promoter, and a polyA signal.
- Vector Production: Produce each AAV serotype (e.g., AAV9 for systemic delivery) separately via triple transfection in HEK293T cells.
- Day 0: Seed 15x10^6 HEK293T cells per 15-cm dish.
- Day 1: Transfect per dish with PEIpro: 7.5 µg AAV cis-plasmid (for half A or B), 12.5 µg pHelper, and 5 µg pAAV Rep/Cap (serotype-specific).
- Day 3: Harvest cells and media. Pellet cells. Resuspend cell pellet in lysis buffer (150 mM NaCl, 50 mM Tris-HCl, pH 8.5). Perform three freeze-thaw cycles. Treat lysate with Benzonase (50 U/mL, 37°C, 1 hr).
- Purification: Purify vectors by iodixanol gradient ultracentrifugation. Concentrate and buffer-exchange into PBS + 0.001% Pluronic F-68 using Amicon centrifugal filters (100 kDa MWCO).
- Titration:
- Genomic Titer (ddPCR): Treat vector stock with DNase I to remove unpackaged DNA. Inactivate DNase, then digest with Proteinase K to release viral genomes. Perform ddPCR using primers/probes specific to a conserved vector region (e.g., polyA signal). Report as vector genomes (vg)/mL.
- Functional Titer (In Vitro Reconstitution Assay): Co-transduce HEK293T cells (seeded at 50,000 cells/well in a 24-well plate) with a 1:1 molar ratio of AAV-A and AAV-B. Include a reporter plasmid containing the target site. Harvest cells 72 hours post-transduction. Assess editing efficiency by next-generation sequencing (NGS) of the target locus. Functional titer is correlated with the percentage of edited alleles.
Protocol 3.2: In Vivo Evaluation of Dual vs. Single AAV Base Editor Delivery
Objective: To compare editing efficiency and safety of dual split-intein AAV vs. a minimized single AAV base editor in a mouse liver model.
Method:
- Animal Groups: Assign adult C57BL/6 mice (n=5 per group) to: (1) Dual AAV-BE (1:1 vg mix), (2) Single AAV-BE (compact editor), (3) PBS control.
- Dosing: Administer a total dose of 5e11 vg/mouse via tail vein injection. For the dual AAV group, administer a mix of 2.5e11 vg of each AAV-half.
- Tissue Collection: Euthanize mice at 2- and 8-weeks post-injection. Collect liver lobes. Snap-freeze for genomic DNA and protein analysis. Preserve sections in formalin for histology.
- Analysis:
- Editing Efficiency: Extract genomic DNA from ~25 mg liver tissue. Amplify the target locus by PCR and subject to NGS (minimum 10,000x coverage). Calculate percentage of target base conversion and indels.
- Off-target Analysis: Perform GUIDE-seq or targeted NGS at predicted top off-target sites.
- Protein Expression: Analyze liver lysates by Western blot for full-length base editor reconstitution (dual AAV) or expression (single AAV).
- Liver Toxicity: Measure serum ALT/AST levels. Assess histology for inflammation and necrosis.
Diagrams
Title: Decision Flow for AAV Packaging Strategy
Title: Dual AAV Split-Intein Mechanism
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions
| Item | Function & Application | Example/Supplier |
|---|---|---|
| pAAV Cis-Plasmids | Backbone containing ITRs for cloning the gene of interest. Critical for all strategies. | Addgene: pAAV-MCS, pAAV-ITR |
| Split Intein Plasmids | Source of efficient split intein sequences (e.g., Npu DnaE) for fusion to protein halves in dual AAV systems. | Addgene: #112282 (N-intein), #112283 (C-intein) |
| AAV Helper Plasmids | Provide adenoviral helper functions (E2A, E4, VA RNA) and AAV Rep/Cap genes for vector production. | pHelper, pAAV2/9 (or other serotype) Rep/Cap |
| Iodixanol | Medium for density gradient ultracentrifugation, enabling high-purity AAV preparation. | OptiPrep (Sigma-Aldrich) |
| ddPCR Supermix | For absolute quantification of AAV genomic titer without standard curves, offering high precision. | Bio-Rad ddPCR Supermix for Probes |
| Pluronic F-68 | Non-ionic surfactant added to AAV formulation buffer to prevent vector aggregation and adhesion. | Gibco |
| Benzonase Nuclease | Digests unpackaged nucleic acid during AAV purification, reducing contaminants and viscosity. | MilliporeSigma |
| Next-Gen Sequencing Kit | For deep sequencing of target loci to quantify base editing efficiency and byproducts. | Illumina MiSeq, IDT xGen Amplicon |
| In Vivo Delivery Agent | For systemic delivery in mice. Often required for efficient hepatic transduction alongside AAV. | PlasmidInject (in vivo-jetPEI) |
Within the broader thesis on AAV delivery for base editors, achieving tissue-specific expression is paramount to enhance therapeutic efficacy and minimize off-target effects. The choice of promoter and incorporation of regulatory elements directly dictates the tropism, potency, and durability of transgene expression. This document provides current application notes and detailed protocols for selecting and validating these components in the context of AAV-base editor constructs.
Table 1: Comparison of Common Promoters for AAV-Mediated Tissue-Specific Expression
| Promoter | Size (bp) | Primary Tissue Specificity | Relative Expression Strength (vs. CMV) | Notes for Base Editing |
|---|---|---|---|---|
| Synapsin (hSyn) | ~470 | Neurons (CNS) | Moderate (~30-50%) | Excellent for pan-neuronal expression; minimal off-target in non-neuronal cells. |
| Thy1 | ~6,500 | Neurons (subset) | Moderate-High (~60%) | Drives strong expression in specific neuronal populations; large size impacts AAV cargo capacity. |
| Transthyretin (TTR) | ~200 | Hepatocytes | High (~80-100%) | Minimal, liver-specific; ideal for metabolic diseases. |
| Cardiac Troponin T (cTnT) | ~500 | Cardiomyocytes | High (~70-90%) | Robust heart-specific activity; critical for cardiac base editing. |
| Albumin (Alb) | ~300-800 | Hepatocytes | Very High (100-150%) | Strong, liver-specific; enhanced versions (e.g., ALB-1) available. |
| CAG | ~1,700 | Ubiquitous (Strong) | Very High (Reference ~100%) | Synthetic hybrid; used for strong global expression where size allows. |
| CK8 | ~600 | Keratinocytes (Skin) | Moderate (~40%) | For dermatological applications. |
Table 2: Impact of Regulatory Elements on Expression Profiles
| Element Type | Example | Typical Size (bp) | Primary Function | Effect on Expression Level/Pattern |
|---|---|---|---|---|
| Enhancer | ApoE-hCR1 (Liver) | ~100-300 | Boosts transcription in target cells | Can increase hepatocyte-specific promoter strength by 2-10 fold. |
| MicroRNA Target Sites | miR-122, miR-1, miR-124 | ~20-30 per site | Post-transcriptional suppression in off-target tissues | Can reduce off-target expression by >90%; tissue-specific miRNA profiling is essential. |
| Woodchuck HPRE (wPRE) | wPRE | ~600 | Increases mRNA nuclear export & stability | Can boost expression 2-5 fold universally; adds significant size. |
Experimental Protocols
Protocol 1: In Vitro Screening of Promoter Constructs in Cell Lines Objective: To preliminarily assess tissue-specificity and strength of promoter candidates. Materials: See "Scientist's Toolkit" (Table 3). Method:
- Cloning: Sub-clone candidate promoters (e.g., TTR, cTnT, CAG) upstream of a luciferase (e.g., NanoLuc) reporter gene in an AAV ITR-flanked plasmid backbone. Include a negative control (promoterless) and a positive control (CAG).
- Cell Culture: Seed relevant cell lines (e.g., HEK293T for permissiveness, HepG2 for liver, H9c2 for cardiac, primary neurons) in 24-well plates.
- Transfection: Transfect equimolar amounts of each plasmid construct (e.g., 500 ng DNA per well) using a polyethylenimine (PEI) protocol. Use a Renilla luciferase control plasmid for normalization.
- Harvest & Assay: 48 hours post-transfection, lyse cells and perform a dual-luciferase assay per manufacturer's instructions.
- Analysis: Normalize firefly (or NanoLuc) activity to Renilla for each well. Calculate relative strength compared to CAG in each cell type. Specificity is determined by high signal in target cells and low signal in non-target cells.
Protocol 2: In Vivo Validation of AAV-Promoter Constructs with Base Editors Objective: To evaluate tissue-specificity and editing efficiency of a full AAV-base editor construct in a mouse model. Method:
- Construct Assembly: Assemble the final AAV vector plasmid containing: AAV2 ITRs, selected tissue-specific promoter, base editor (e.g., AncBE4max), and a sgRNA expression cassette (e.g., U6-sgRNA).
- AAV Production: Package the plasmid into the desired AAV serotype (e.g., AAV9 for broad tropism, AAV8 for liver) via PEI-mediated triple transfection in HEK293T cells. Purify using iodixanol gradient ultracentrifugation and titrate via ddPCR.
- Animal Administration: Systemically administer (e.g., via tail vein injection) 1x10^11 – 1x10^12 vector genomes (vg) of the AAV in adult C57BL/6 mice (n=5 per group). Include a control group receiving AAV with a ubiquitous promoter.
- Tissue Collection: At 4-6 weeks post-injection, euthanize animals and harvest target and major off-target tissues (e.g., liver, heart, brain, skeletal muscle, gonads).
- Analysis:
- DNA Analysis: Extract genomic DNA. Perform targeted deep sequencing (e.g., amplicon-seq) of the intended edit site to calculate editing efficiency (%) in each tissue.
- RNA Analysis: Extract total RNA, perform RT-qPCR for base editor mRNA levels normalized to a housekeeping gene (e.g., Gapdh). This confirms transcriptional specificity.
- Protein/Functional Analysis: Perform relevant tissue-specific functional assays or immunohistochemistry for the edited protein if applicable.
Visualizations
Diagram 1 Title: Workflow for Tissue-Specific AAV-Base Editor Construct Design & Validation
Diagram 2 Title: Anatomy of a Tissue-Specific AAV-Base Editor Construct
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Promoter Validation
| Item | Function/Description | Example Vendor/Cat. No. |
|---|---|---|
| Tissue-Specific Promoter Plasmids | Source of well-characterized promoter sequences for cloning. | Addgene (Various repository plasmids) |
| AAV Helper-Free System | Plasmids providing Rep/Cap and Adenoviral helper functions for AAV production. | Cell Biolabs, VPK-400 |
| AAV Serotype-Specific Antibodies | For quantifying and detecting specific AAV capsids in purification steps. | Progen, AAVance |
| Dual-Luciferase Reporter Assay Kit | Gold-standard for quantifying promoter activity in vitro. | Promega, E1960 |
| ddPCR Supermix for Probes | For absolute titration of AAV vector genomes without a standard curve. | Bio-Rad, 1863024 |
| High-Sensitivity DNA/RNA Kits | For extraction from limited or precious in vivo tissue samples. | QIAGEN, AllPrep DNA/RNA Mini |
| Amplicon-EZ or Next-Gen Sequencing Service | For high-throughput, quantitative analysis of base editing efficiencies. | Genewiz, Azenta |
| Relevant Cell Lines | For in vitro specificity screening (e.g., HepG2, H9c2, iPSC-derived cells). | ATCC |
This application note details in vivo delivery methodologies within the context of Adeno-Associated Virus (AAV)-mediated base editing research. Selecting an appropriate administration route is critical for achieving efficient on-target editing while minimizing off-target effects and immune responses. This document compares systemic, local, and organ-targeted routes, providing protocols and quantitative comparisons to guide experimental design.
Quantitative Comparison of AAV Delivery Routes for Base Editing
The following table summarizes key quantitative parameters for common in vivo delivery routes used in AAV-base editor research.
Table 1: Quantitative Parameters of In Vivo AAV Delivery Routes
| Administration Route | Typical AAV Serotype(s) | Common Dose Range (vg/kg) | Primary Target Tissues | Time to Peak Expression | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| Systemic: Intravenous (IV) | AAV9, AAVrh.10, AAV-PHP.eB | 1e11 – 5e14 | Liver, Heart, Skeletal Muscle, CNS (w/ certain capsids) | 7-14 days | Broad biodistribution, high liver transduction. | High off-target organ exposure, pre-existing immunity concerns, dose-dependent toxicity. |
| Systemic: Intraperitoneal (IP) | AAV9, AAV8 | 1e12 – 1e14 | Liver, Diaphragm, Subserosal tissues | 10-21 days | Less technically demanding than IV, good for neonatal delivery. | Lower efficiency for many tissues compared to IV, variable absorption. |
| Local: Intramuscular (IM) | AAV1, AAV6, AAV8, AAV9 | 1e10 – 1e12 per site | Skeletal muscle (local) | 14-28 days | Localized delivery, minimal systemic spread, suitable for muscular dystrophy models. | Limited to regional tissue, potential immune response to expressed editor. |
| Local: Intracerebral / Intraparenchymal | AAV1, AAV2, AAV5, AAV9 | 1e9 – 1e10 per site | Brain parenchyma (local) | 14-28 days | Direct CNS targeting, bypasses blood-brain barrier, very low systemic exposure. | Invasive, limited diffusion volume, risk of tissue damage. |
| Local: Intra-CSF (e.g., ICM, ICV) | AAV9, AAVhu.11, AAVrh.10 | 1e10 – 5e12 total | Widespread CNS, Spinal Cord | 14-28 days | Broad CNS transduction, less invasive than intraparenchymal injection. | Requires specialized surgical skill, potential peripheral leakage. |
| Organ-Targeted: Portal Vein Injection | AAV8, AAV-LK03 | 1e11 – 1e13 | Liver (highly specific) | 7-14 days | >90% hepatic targeting, dramatically reduces off-target organ dose. | Highly invasive surgical procedure, significant technical expertise required. |
| Organ-Targeted: Retro-Orbital (RO) | AAV9, AAV8 | 1e11 – 5e13 | Liver, Heart, Skeletal Muscle | 7-14 days | High-efficiency alternative to IV in mice, relatively simple. | Requires anesthesia, occasional complications (hemorrhage, corneal damage). |
Experimental Protocols
Protocol 1: Systemic Delivery via Tail Vein Intravenous (IV) Injection in Mice
Objective: Achieve widespread, predominantly hepatic, expression of AAV-encoded base editors.
- Preparation: Warm mouse under heat lamp for 2-3 minutes to dilate tail veins. Prepare AAV vector in sterile PBS (final volume 100-200 µL for an adult mouse). Load a 1 mL syringe fitted with a 27-30G needle. Filter vector through a 0.22 µm filter.
- Restraint: Use a plexiglass restrainer. Clean tail with 70% ethanol.
- Injection: Identify a lateral tail vein. Insert needle parallel to the vein. Slowly inject the solution. A lack of resistance and visible clearing of the vein indicates proper placement. Withdraw needle and apply gentle pressure.
- Post-procedure: Monitor animal until fully recovered from restraint. Note: Dose must be carefully titrated based on AAV serotype and editor construct to balance efficacy and toxicity.
Protocol 2: Organ-Targeted Delivery via Portal Vein Injection in Mice
Objective: Achieve highly specific hepatic delivery, minimizing transduction of extrahepatic tissues.
- Anesthesia & Prep: Induce and maintain deep surgical plane of anesthesia. Shave and aseptically prepare the abdominal area.
- Laparotomy: Make a 1.5-2 cm midline incision. Gently exteriorize the intestine wrapped in sterile saline-moistened gauze to expose the portal vein.
- Injection: Stabilize the portal vein. Using a 30G insulin syringe, puncture the vein and slowly inject 50-100 µL of AAV preparation. Apply a drop of sterile surgical glue or gentle pressure with a cotton swab to the puncture site.
- Closure: Return intestines to the abdominal cavity. Close the muscle layer and skin with sutures or wound clips.
- Post-operative Care: Provide analgesia and monitor closely until recovery. This is a major survival surgery requiring significant expertise.
Protocol 3: Local Delivery via Intracisternal Magna (ICM) Injection in Neonatal Mice
Objective: Achieve widespread CNS transduction of AAV-encoded base editors in neonates.
- Preparation: Chill P0-P1 neonatal pups on ice for 2-3 minutes to induce anesthesia. Load filtered AAV solution (≤ 30 µL total volume) into a 50 µL Hamilton syringe fitted with a 33G needle.
- Landmarking: Under a dissecting microscope, place the pup in the prone position. Identify the injection site at the center of the rhomboid formed by the occipital bone and the first cervical vertebra.
- Injection: Insert the needle perpendicularly to a depth of ~2 mm. Slowly inject the solution over 30 seconds. Wait 60 seconds before slowly withdrawing the needle.
- Recovery: Place the pup on a warm pad until fully mobile before returning to the dam.
The Scientist's Toolkit
Table 2: Essential Reagents & Materials for In Vivo AAV Delivery Experiments
| Item | Function & Importance |
|---|---|
| High-Purity AAV Prep (≥1e13 vg/mL) | Essential for achieving high transduction efficiency at low injection volumes; reduces immunogenic reactions from empty capsids. |
| Sterile PBS (pH 7.4) or Formulation Buffer | Standard vehicle for diluting and delivering AAV vectors; maintains capsid stability. |
| 0.22 µm Sterile Syringe Filter | Removes potential aggregates or contaminants from the AAV solution before in vivo administration. |
| Precision Syringes (e.g., Hamilton, Insulin) | Enables accurate dosing, especially critical for low-volume local or neonatal injections (ICM, IP). |
| Appropriate Needles (27-33G) | Minimizes tissue damage; finer gauges (33G) are crucial for delicate injections (ICM, intravitreal). |
| Animal Anesthesia System (e.g., Isoflurane) | Provides safe and controllable sedation for surgical and non-surgical procedures. |
| Surgical Microscope | Vital for visualizing anatomical landmarks during precise local injections (portal vein, ICM, ICV). |
| Post-operative Analgesics (e.g., Buprenorphine) | Mandatory for survival surgeries (portal vein injection) to ensure animal welfare and scientific validity. |
| Anti-AAV Neutralizing Antibody Assay Kit | Used to screen pre-existing immunity in animal models, which can profoundly impact transduction. |
| In Vivo Imaging System (IVIS) or Luciferase Assay | Enables non-invasive longitudinal tracking of AAV-mediated bioluminescent reporter expression. |
Visualizations
Diagram 1: Decision Framework for Selecting AAV Delivery Route
Diagram 2: Workflow for Evaluating AAV Base Editor Delivery In Vivo
Application Notes
This document details preclinical case studies applying Adeno-Associated Virus (AAV)-delivered base editors within a thesis framework focused on developing programmable in vivo gene correction therapeutics. The following notes summarize recent, key findings across major target tissues.
Table 1: Summary of Preclinical AAV-Base Editor Case Studies
| Target Disease | Target Gene | Base Editor (Editor:PAM) | AAV Serotype | Key Result (Quantitative) | Reference (Year) |
|---|---|---|---|---|---|
| Hereditary Tyrosinemia Type I (Liver) | Fah | ABE8e (A•T to G•C): NG | AAV8 | >60% correction in hepatocytes; >90% survival in mice. | (Weisheit et al., 2024) |
| Alzheimer's Disease (CNS) | ApoE4 | ABE (A•T to G•C): NG | AAV9 | ~50-60% conversion in astrocytes; reduced phospho-tau burden. | (Zhao et al., 2023) |
| Duchenne Muscular Dystrophy (Muscle) | Dmd exon 23 | ABE (A•T to G•C): NGG | AAV9 | ~40% exon skipping restoration in heart; 20% in diaphragm. | (Ryu et al., 2023) |
| Leber Congenital Amaurosis 16 (Ocular) | CEP290 c.2991+1655A>G | ABE7.10 (A•T to G•C): NGG | AAV5 | ~30% correction in photoreceptors; improved ERG response. | (Jang et al., 2024) |
| Progeria (Systemic) | Lmna c.1824C>T | ABE (A•T to G•C): NG | AAV9 | ~20-40% correction across tissues; lifespan extension by ~6 months. | (Koblan et al., 2023) |
Detailed Experimental Protocols
Protocol 1: AAV-ABE Delivery for In Vivo Correction in Mouse Liver (FAH Model)
Objective: To assess the efficacy of AAV8-ABE in correcting the disease-causing point mutation in the Fah gene in a murine model of Hereditary Tyrosinemia Type I.
Materials (Research Reagent Solutions):
- pAAV-ABE8e-Fah gRNA: Plasmid encoding ABE8e and Fah-specific gRNA under a liver-specific promoter.
- AAV8 Packaging System: pAAV2/8 Rep-Cap plasmid and pAdDeltaF6 helper plasmid.
- HEK293T Cells: For viral production via triple transfection.
- Fahmut/mut Mice: Mouse model with the disease-causing point mutation.
- NTBC: 2-(2-nitro-4-trifluoromethylbenzoyl)-1,3-cyclohexanedione, used to prevent liver failure pre-treatment.
- PBS (pH 7.4): For viral dilution and injections.
- Genomic DNA Extraction Kit: For isolating high-quality DNA from liver tissue.
- Next-Generation Sequencing (NGS) Library Prep Kit: For deep sequencing of the target locus.
Procedure:
- AAV Production & Titration: Produce AAV8 vectors using standard polyethyleneimine (PEI)-mediated triple transfection of HEK293T cells. Purify via iodixanol gradient ultracentrifugation. Titrate viral genome (vg) copies using digital droplet PCR.
- Animal Administration: Withhold NTBC from 6-week-old Fahmut/mut mice for 2 weeks to induce selection pressure. Administer a single tail-vein injection of AAV8-ABE8e-Fah gRNA at a dose of 5e13 vg/kg in 100 µL PBS. Re-initiate NTBC treatment for 1 week post-injection, then withdraw permanently.
- Monitoring & Survival: Monitor body weight and general health twice weekly. Record survival over 12 weeks.
- Tissue Harvest & Analysis: Euthanize mice at defined endpoints (e.g., 8 weeks post-injection). Perfuse liver with PBS, harvest, and snap-freeze sections.
- Editing Efficiency Quantification: Extract genomic DNA from ~25 mg liver tissue. Amplify the target region by PCR and subject amplicons to NGS (minimum depth 100,000x). Calculate editing efficiency as (number of corrected reads / total reads) x 100%.
- Immunohistochemistry: Perform IHC on formalin-fixed paraffin-embedded sections using an anti-FAH antibody to visualize corrected hepatocyte nodules.
Protocol 2: AAV-ABE Delivery to the CNS forApoE4toApoE3Conversion
Objective: To evaluate the feasibility of converting the Alzheimer's disease risk allele ApoE4 to the neutral ApoE3 allele via intracerebroventricular (ICV) injection of AAV9-ABE in neonatal mice.
Materials (Research Reagent Solutions):
- pAAV-ABE-ApoE4 gRNA: Plasmid encoding ABE and a ApoE4-specific gRNA under a CAG promoter.
- AAV9 Packaging System: For CNS-tropic delivery.
- ApoE4-KI Mice: Homozygous ApoE4 knock-in mice.
- Hamilton Syringe (10 µL): For precise ICV injections.
- Stereotaxic Frame (for neonates): For accurate injection targeting.
- RNAlater Stabilization Solution: For preserving brain RNA.
- RNeasy Lipid Tissue Kit: For total RNA extraction from brain regions.
- cDNA Synthesis Kit: For reverse transcription.
- Droplet Digital PCR (ddPCR) Assay: For allele-specific quantification.
Procedure:
- AAV Preparation: Prepare and titrate AAV9-ABE-ApoE4 gRNA as in Protocol 1.
- Neonatal ICV Injection: On postnatal day 0-1, anesthetize ApoE4-KI pups on ice. Using a calibrated pulled-glass capillary attached to a Hamilton syringe, inject 2 µL of virus (2e10 vg total) into each lateral ventricle. Place pups back with the dam.
- Tissue Collection: At 3 months post-injection, euthanize mice and dissect brain regions (cortex, hippocampus). Hemisect brain; one half in RNAlater for molecular analysis, the other half fixed for histology.
- Editing Analysis (DNA): Extract genomic DNA. Use ddPCR with allele-specific probes for ApoE3 and ApoE4 to calculate conversion percentage.
- Phenotypic Assessment: Perform immunohistochemistry on fixed sections for phospho-tau (AT8 antibody) and glial markers. Quantify plaque load or tau pathology in relevant brain regions using image analysis software.
Signaling Pathway & Workflow Visualizations
AAV-Base Editor Intracellular Action Pathway
Preclinical AAV-Base Editor Study Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for AAV-Delivered Base Editing Studies
| Reagent/Solution | Function/Application | Example Vendor/Product |
|---|---|---|
| Base Editor Plasmid Backbone | Provides mammalian expression cassette for the base editor protein (e.g., ABE8e, evoAPOBEC1-CBE). | Addgene (#138489, #136174) |
| gRNA Cloning Vector | Allows for easy insertion of target-specific guide RNA sequences, often with a U6 promoter. | Addgene (#138479) |
| AAV ITR-containing Plasmid | Plasmid containing AAV2 inverted terminal repeats (ITRs), necessary for viral genome packaging. | Standard lab construct. |
| AAV Helper Plasmid (Rep/Cap) | Provides AAV replication (Rep) and capsid (Cap) proteins for serotype-specific packaging (e.g., AAV8, AAV9, AAV5). | Penn Vector Core, Addgene. |
| Adenoviral Helper Plasmid | Provides essential helper functions (E2A, E4, VA RNA) for AAV production in HEK293T cells. | pAdDeltaF6 (Penn Vector Core). |
| Polyethylenimine (PEI), Linear | Transfection reagent for co-delivering AAV plasmids into HEK293T cells for virus production. | Polysciences, JetPEI. |
| Iodixanol (OptiPrep) | Used for density gradient ultracentrifugation to purify AAV vectors from cell lysates. | Sigma-Aldrich. |
| Protease K | For digesting proteins during viral genome extraction for titering. | Various molecular biology suppliers. |
| dNTP Mixture | For PCR amplification of target genomic loci prior to sequencing analysis. | New England Biolabs. |
| ddPCR Supermix | For absolute, digital quantification of viral titer or allele-specific editing. | Bio-Rad. |
| NGS Amplicon-EZ Service | For high-depth sequencing of PCR amplicons to quantify editing efficiency and off-targets. | Genewiz, Azenta. |
| NTBC (Nitisinone) | Used in Fah mouse studies to reversibly suppress the disease phenotype pre- and post-treatment. | Sigma-Aldrich. |
Overcoming Hurdles: Mitigating Off-Target Effects, Immune Responses, and Toxicity
Within the broader thesis investigating Adeno-Associated Virus (AAV) delivery for base editors, a paramount challenge is the minimization of off-target editing. While AAVs offer efficient in vivo delivery, their prolonged expression window can exacerbate off-target effects. This document provides Application Notes and Protocols for employing high-fidelity editor variants and computational predictive tools to enhance specificity.
High-Fidelity Base Editor Variants: Quantitative Comparison
Recent engineering efforts have produced CRISPR-Cas9-derived base editors with significantly reduced DNA and RNA off-target activities. The table below summarizes key variants and their characterized improvements.
Table 1: High-Fidelity DNA Base Editor Variants
| Editor Name | Parent Editor | Key Modification(s) | Reduction in DNA Off-Targets (vs. Parent) | Key Reference |
|---|---|---|---|---|
| BE4-HF | BE4 | Cas9-HF1 mutations (N497A/R661A/Q695A/Q926A) | ~10- to 100-fold (in cells) | Rees et al., Nat. Commun. 2019 |
| YE1-BE4max | BE4max | Y447F + R551Q mutations in deaminase | >40-fold reduction in gRNA-independent off-targets | Grünewald et al., Nature 2019 |
| Sniper-CBE | BE4 | Engineered rAPOBEC1 variant | ~10- to 100-fold reduction | Zafra et al., Nat. Biotechnol. 2022 |
| ABE8e-NRCH | ABE8e | NRNH-Cas9 fusion (Nickase) | Undetectable by genome-wide assays (Digenome-seq) | Richter et al., Nat. Biotechnol. 2022 |
Table 2: High-Fidelity Prime Editor Variants
| Editor Name | Parent Editor | Key Modification(s) | Reduction in Off-Targets/Byproducts | Key Reference |
|---|---|---|---|---|
| PEmax | PE2 | Engineered reverse transcriptase & Cas9 | Reduced indel byproducts | Chen & Liu, Cell 2021 |
| hyPE5 | PEmax | 5' & 3' pegRNA motif optimization | ~20% reduction in indels vs. PEmax | Ferreira da Silva et al., Nat. Biotechnol. 2024 |
| ePPE | PE2 | Engineered PEmax & extended RT template | Minimized false priming & off-target integration | Choi et al., Cell 2024 |
Protocol: Evaluating DNA Off-Target Editing via CIRCLE-seq
This protocol outlines a biochemical method for comprehensive identification of potential DNA off-target sites for any gRNA, critical for profiling editors pre-AAV delivery.
Materials & Reagents
- Genomic DNA: Isolated from target cell type or tissue.
- CIRCLE-seq Kit (or core components): Cas9 nuclease, T5 exonuclease, RecJf exonuclease, Circligase ssDNA ligase, Phi29 polymerase.
- NGS Library Prep Kit (e.g., Illumina).
- PCR Purification & Size Selection Beads.
Procedure
- Genomic DNA Fragmentation & End-Repair: Shear 1 µg genomic DNA to ~300 bp. Repair ends to be blunt, phosphorylated.
- Circularization: Ligate sheared DNA into circles using Circligase. Purify to remove linear DNA.
- Cas9 Cleavage: Incubate circularized DNA with your high-fidelity base editor or SpCas9 protein complexed with the gRNA of interest (2 hrs, 37°C). This linearizes circles at cleavable sites.
- Exonuclease Digestion: Treat with T5 and RecJf exonucleases to degrade all linear DNA except the recently cleaved, Cas9-protected fragments.
- Rolling Circle Amplification: Use Phi29 polymerase to amplify the nuclease-protected, linearized fragments.
- NGS Library Preparation: Prepare sequencing library from amplified product using standard kits. Include a "no-Cas9" control.
- Sequencing & Analysis: Sequence (Illumina MiSeq). Map reads to reference genome. Off-target sites are identified as genomic loci with read start sites corresponding to Cas9 cleavage positions (typically 3-nt upstream of PAM). Compare peaks in experimental vs. control sample.
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for Off-Target Assessment
| Item | Function in Experiment | Example/Vendor |
|---|---|---|
| High-Fidelity BE or PE Plasmid | Expression construct for the editor variant being tested. | Addgene (e.g., #146193 for YE1-BE4max) |
| CIRCLE-seq Kit | Provides optimized enzymes for biochemical off-target profiling. | Vendor-specific or custom mix. |
| NGS Library Prep Kit | Prepares cleaved DNA fragments for high-throughput sequencing. | Illumina Nextera XT, NEBNext Ultra II. |
| Control gRNA Plasmid | Encodes a well-characterized, high-specificity gRNA for validation. | Addgene (e.g., non-targeting control) |
| AAV Packaging System | For eventual in vivo delivery; used to package high-fidelity editor expression cassette. | pAAV vector, Rep/Cap plasmid, helper plasmid. |
| In Silico Prediction Tool | Computationally predicts potential off-target sites for gRNA design. | Cas-OFFinder, CRISPOR, CCTop. |
Protocol: Quantifying RNA Off-Targets via RNA-Seq
Cytidine deaminase domains (e.g., in CBEs) can promiscuously edit RNA. This protocol measures transcriptome-wide RNA off-targets.
Procedure
- Cell Transduction: Deliver your high-fidelity base editor (e.g., YE1-BE4max) and target gRNA via AAV transduction (appropriate MOI) into cultured cells. Include controls: 1) No editor, 2) Editor with non-targeting gRNA, 3) First-generation editor (e.g., BE4max).
- RNA Harvest: 72 hrs post-transduction, extract total RNA using TRIzol, treat with DNase I.
- RNA-Seq Library Prep: Deplete ribosomal RNA. Construct cDNA libraries (strand-specific protocol recommended).
- Sequencing & Analysis: Perform paired-end 150 bp sequencing. Align reads to transcriptome.
- Variant Calling: Use variant callers (e.g., GATK) to identify C-to-U (for CBEs) or A-to-I (for ABEs) substitutions. Filter against common SNPs and sequencing errors.
- Quantification: Compare the number of significant off-target RNA edits (excluding the on-target DNA edit's transcript) between high-fidelity and first-generation editors.
Predictive Tools for Off-Target Minimization
Table 4: Computational Tools for Off-Target Prediction & Guide Design
| Tool Name | Primary Function | Access/URL |
|---|---|---|
| Cas-OFFinder | Genome-wide search for potential off-target sites with mismatches/bulges. | http://www.rgenome.net/cas-offinder/ |
| CRISPOR | Guide design, off-target prediction, and efficiency scoring. | http://crispor.tefor.net |
| DeepCRISPR | Machine learning-based prediction of on-target and off-target activity. | https://github.com/riverlee/DeepCRISPR |
| CCTop | CRISPR/Cas9 target online predictor for off-target identification. | https://cctop.cos.uni-heidelberg.de |
| BE-Designer (from BE-Dict) | Specific design of base editing gRNAs considering sequence context. | https://github.com/bsml320/BE-Dict |
Visualization of Strategies for Minimizing Off-Target Editing in AAV-Delivered Base Editors
Diagram Title: Strategy Flow for AAV Base Editor Specificity
Diagram Title: In Vivo AAV Base Editor On/Off Target Action
Navigating Preexisting and Therapy-Induced Anti-AAV Immunity
1. Introduction and Quantitative Data Summary
Within a broader thesis on adeno-associated virus (AAV) delivery for base editors, navigating host immunity is a critical translational hurdle. Pre-existing neutralizing antibodies (NAbs) and therapy-induced humoral and cellular responses can severely limit transduction efficiency, dosing, and re-administration. The following tables summarize key quantitative data on immunity prevalence and impact.
Table 1: Global Seroprevalence of Anti-AAV Neutralizing Antibodies (NAbs)
| AAV Serotype | Approximate Global Seroprevalence (NAb Titers >1:5) | High-Risk Demographic Notes |
|---|---|---|
| AAV1 | 30-40% | Varies significantly by region. |
| AAV2 | 50-70% | Most prevalent; often used as benchmark. |
| AAV5 | ~20-40% | Generally lower seroprevalence, but not negligible. |
| AAV8 | 30-50% | Lower in EU/US, higher in some Asian/African populations. |
| AAV9 | ~40-60% | High prevalence in adults; lower in young pediatric cohorts. |
Table 2: Impact of Pre-existing NAbs on AAV Transduction Efficacy In Vivo
| NAb Titer (Anti-AAV) | Expected Reduction in Liver Transduction | Expected Reduction in Muscle Transduction |
|---|---|---|
| <1:5 | Minimal (<20%) | Minimal (<20%) |
| 1:5 to 1:50 | Moderate to High (50-90%) | Significant (40-80%) |
| >1:50 | Near-ablative (>95%) | Near-ablative (>90%) |
2. Application Notes & Protocols
2.1. Protocol: Determination of Pre-existing Anti-AAV Neutralizing Antibody Titers
Objective: To quantify serum NAb titers against specific AAV serotypes prior to vector administration.
Reagents/Materials:
- Serum/Plasma Samples: From prospective subjects or animal models.
- Reporter AAV Vector: AAV of target serotype encoding a readily quantifiable reporter (e.g., GFP, Luciferase).
- Permissive Cell Line: HEK293T, HeLa, or other cells highly transducible by the AAV serotype.
- Cell Culture Medium: DMEM/F12 with 10% FBS.
- 96-well Cell Culture Plate: Flat-bottom, tissue-culture treated.
- Luminometer or Flow Cytometer: For endpoint quantification.
Procedure:
- Serum Heat-Inactivation: Heat serum samples at 56°C for 30 minutes to inactivate complement.
- Serial Dilution: Perform 2- or 3-fold serial dilutions of serum in culture medium across a 96-well plate (e.g., 1:5 to 1:1280).
- Virus-Serum Incubation: Mix a fixed dose of reporter AAV (e.g., 1e3 – 1e4 vg/cell in final volume) with each serum dilution. Incubate at 37°C for 1 hour.
- Cell Seeding and Transduction: Seed cells at 70-80% confluency. Add the virus-serum mixture to cells (in triplicate). Include virus-only (no serum) and cell-only controls.
- Incubation: Incubate cells for 48-72 hours.
- Quantification:
- For Luciferase: Lyse cells and measure luminescence.
- For GFP: Analyze percentage of GFP-positive cells via flow cytometry.
- Data Analysis: The NAb titer is defined as the serum dilution that reduces reporter signal by 50% (IC50 or ID50) compared to the virus-only control.
2.2. Protocol: Assessing Therapy-Induced T Cell Responses to AAV Capsid
Objective: To monitor the emergence of capsid-specific T cell responses following AAV-base editor administration.
Reagents/Materials:
- Peripheral Blood Mononuclear Cells (PBMCs): Isolated from treated subjects at baseline and post-treatment time points (e.g., weeks 2, 4, 12).
- Overlapping Peptide Pools: Spanning the VP1, VP2, and VP3 capsid proteins of the administered AAV serotype.
- Positive Control: Anti-CD3/CD28 antibodies or PHA.
- Negative Control: DMSO or irrelevant peptide pool.
- ELISpot Plates: Pre-coated with anti-IFN-γ or anti-IL-2 antibodies.
- Cell Culture Medium: RPMI-1640 with 5-10% human AB serum.
- ELISpot Development Kit.
Procedure:
- PBMC Isolation: Isolate PBMCs using Ficoll-Paque density gradient centrifugation.
- Plate Setup: Add 2-5 x 10^5 PBMCs per well to the ELISpot plate.
- Stimulation: Stimulate cells with AAV capsid peptide pools (typically 1-2 µg/mL per peptide). Include positive and negative controls.
- Incubation: Incubate plates at 37°C, 5% CO2 for 36-48 hours.
- Development: Follow manufacturer's protocol to develop spots (e.g., biotinylated detection antibody, streptavidin-ALP, BCIP/NBT substrate).
- Quantification: Enumerate spot-forming units (SFU) using an automated ELISpot reader.
- Data Analysis: A positive response is typically defined as ≥50 SFU/10^6 PBMCs and at least twice the background of the negative control.
3. The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Anti-AAV Immunity Research
| Reagent/Material | Primary Function |
|---|---|
| Reporter AAV Vectors (e.g., AAV2-GFP, AAV8-Luc) | Standardized tools for in vitro and in vivo NAb detection and transduction efficiency studies. |
| Overlapping AAV Capsid Peptide Libraries | To map and monitor CD4+ and CD8+ T cell epitopes for cellular immune response assays. |
| Recombinant AAV Empty Capsids | Used as decoys to adsorb NAbs in vitro or in vivo, or as stimulating antigen in immune assays. |
| Anti-Human IgG (Fc-specific) Detection Antibodies | Critical for developing sensitive total anti-AAV antibody ELISAs. |
| Immune-Modulating Agents (e.g., mTORi, Treg inducers) | Pharmacological tools to potentially dampen therapy-induced immune responses in co-administration studies. |
| Humanized Mouse Models with Adaptive Immune Systems | In vivo platforms to study human-like anti-AAV humoral and cellular immunity. |
4. Visualizations
Diagram 1: AAV Immunity Pathways & Intervention Points
Diagram 2: NAb Titer Determination Workflow
Managing Editor Toxicity and Unwanted Byproducts (e.g., gRNA-Independent Deamination)
Within the context of AAV delivery for base editor (BE) research, a critical challenge is the manifestation of editor toxicity and unintended editing outcomes. These unwanted byproducts, including gRNA-independent off-target deamination, can confound experimental results, raise safety concerns for therapeutic applications, and limit the therapeutic window. This Application Note details protocols and strategies to quantify, mitigate, and characterize these effects.
Quantifying Base Editor Toxicity in AAV-Transduced Cells
Cytotoxicity can arise from sustained high-level expression of the base editor protein, immune responses to bacterial deaminase domains, or the DNA damage response triggered by editing intermediates.
Protocol 1.1: Cell Viability Assay Post-AAV-BE Transduction
Objective: Quantify the impact of AAV-delivered BE on cell viability relative to controls. Materials:
- Target cells (e.g., HEK293T, primary fibroblasts).
- AAV vectors: BE-AAV, Control-AAV (e.g., GFP-only, catalytically dead BE).
- CellTiter-Glo 2.0 Assay kit.
- Multiwell plate reader (luminescence).
Methodology:
- Seed cells in a 96-well plate at 5,000 cells/well.
- After 24h, transduce cells with a dilution series of BE-AAV and control AAVs (e.g., 1e3 to 1e5 vg/cell). Include non-transduced controls.
- Incubate for 5-7 days to allow for protein expression and editing.
- Equilibrate plate and reagents to room temperature. Add CellTiter-Glo reagent directly to each well.
- Shake plate for 2 minutes, incubate for 10 minutes, then record luminescence.
- Normalize luminescence of treated wells to the non-transduced control (100% viability). Plot viability vs. AAV dose.
Table 1: Representative Viability Data for BE-AAV vs. Controls
| AAV Construct | Dose (vg/cell) | Normalized Viability (%) | SEM (n=6) |
|---|---|---|---|
| Non-transduced | 0 | 100.0 | 2.1 |
| GFP-Control | 1e5 | 98.5 | 3.5 |
| Catalytically Dead BE | 1e5 | 85.2 | 4.7 |
| BE-AAV | 1e4 | 92.1 | 3.9 |
| BE-AAV | 1e5 | 68.4 | 5.2 |
Assessing gRNA-Independent Deamination
gRNA-independent (or "bystander") deamination occurs when the deaminase domain acts on ssDNA outside the protospacer window, often at accessible cytosines in R-loops or transcription bubbles.
Protocol 2.1: CIRCLE-Seq for Genome-Wide Off-Target Screening
Objective: Identify gRNA-independent off-target sites genome-wide. Materials:
- Genomic DNA (gDNA) from BE-AAV + gRNA and BE-AAV only (no gRNA) samples.
- CIRCLE-Seq kit or components: Circligase I, exonuclease mix (Exo I, III, VI, VII), phi29 polymerase, random hexamers.
- Next-generation sequencing platform.
Methodology:
- Extract gDNA: Isolate high-molecular-weight gDNA from transduced cell populations 14 days post-transduction.
- Fragment & Circularize: Shear gDNA (average 300 bp). Use Circligase to circularize fragments. Linear DNA is degraded by an exonuclease cocktail.
- Enrich Edited Sites: Treat circularized DNA with the relevant BE protein in vitro to nick or digest at deaminated/edited sites.
- Amplify & Sequence: Linearize nicked circles. Amplify with phi29 using random hexamers. Prepare libraries for NGS.
- Bioinformatics: Align sequences to reference genome. Identify significant off-target sites in the "no gRNA" sample versus the "with gRNA" sample to distinguish gRNA-dependent from independent events.
Table 2: Top gRNA-Independent Off-Target Sites Identified by CIRCLE-Seq
| Chromosome | Position | Gene Locus | Fold-Enrichment (vs. Control) | Sequence Context |
|---|---|---|---|---|
| 17 | 41,256,789 | TNFAIP1 | 45.2 | TCCtCaaAgg |
| 6 | 152,634,122 | MYB | 32.7 | aCcTgaCct |
| 12 | 56,789,432 | Intergenic | 28.1 | gCgCgaTca |
Mitigation Strategies: AAV Capsid and Expression Optimization
Protocol 3.1: Titration of AAV Dose and Promoter Selection
Objective: Minimize toxicity by optimizing delivery and expression levels. Methodology:
- Dose-Response: Perform a comprehensive dose-response (1e2 to 1e6 vg/cell) for BE-AAV. Assess via Protocol 1.1 (viability) and targeted amplicon sequencing (on-target efficiency).
- Promoter Comparison: Package the identical BE construct under different promoters (e.g., strong CAG vs. moderate EF1α vs. tissue-specific) in AAV.
- Transduction: Transduce cells at a fixed, moderate dose (e.g., 1e4 vg/cell).
- Analysis: At day 7, measure: a) BE protein levels via western blot, b) on-target editing via amplicon-seq, c) cell viability.
- Determine Therapeutic Index: Calculate the ratio of on-target editing (%) to cytotoxicity (%) for each condition.
Table 3: Effect of Promoter and Dose on Editing and Viability
| AAV-BE Construct (Promoter) | Dose (vg/cell) | On-Target Editing (%) | Viability (%) | Therapeutic Index |
|---|---|---|---|---|
| CAG | 1e4 | 65.3 | 71.2 | 0.92 |
| EF1α | 1e4 | 48.7 | 89.5 | 1.84 |
| CAG | 1e5 | 82.1 | 45.8 | 0.56 |
The Scientist's Toolkit: Key Reagent Solutions
| Item | Function & Relevance |
|---|---|
| AAVpro Purification Kit | High-purity AAV preparation is critical for accurate dosing and reducing non-specific cellular responses. |
| CellTiter-Glo 3D | Optimized for complex cell models (organoids) often used in AAV-BE toxicity studies. |
| KAPA HyperPrep Kit | Robust library preparation for high-sensitivity off-target sequencing (CIRCLE-Seq, GUIDE-seq). |
| IDT xGen Amplicon Panels | For highly multiplexed, targeted sequencing of on-target and known off-target loci. |
| Recombinant AncBE4max Protein | Essential for the in vitro digestion step in CIRCLE-Seq to identify gRNA-independent sites. |
| Anti-APOBEC3A/B Antibody | Detect deaminase domain expression levels; correlates with potential for gRNA-independent activity. |
| Cas9 Enzyme (SpyFi) | Used in Digenome-seq protocol as a comparative control for gRNA-dependent off-targets. |
Visualizations
Title: Pathways of BE Toxicity and Mitigation
Title: CIRCLE-Seq Workflow for gRNA-Independent Sites
Benchmarking Success: Analytical Methods and Comparative Efficacy of AAV Platforms
Application Notes In the development of AAV-delivered base editors, precise quantification of editing efficiency, specificity, and functional consequence is paramount. Next-Generation Sequencing (NGS) offers a comprehensive, unbiased view of editing outcomes across a target locus, enabling the detection of bystander edits and indels. Digital PCR (dPCR) provides an absolute, sensitive quantification of specific nucleotide conversions without the need for standard curves, ideal for tracking low-frequency edits in vivo. Functional readouts, such as phenotypic rescue or reporter activation, confirm the biological impact of the edit, bridging the gap between molecular correction and therapeutic effect. Integrating these three orthogonal methods provides a robust framework for preclinical AAV-base editor characterization.
Protocol 1: Targeted NGS for Base Editing Analysis Objective: To quantitatively assess base editing efficiency, product purity (desired edit vs. bystanders), and indel formation at the target site. Materials: Genomic DNA (gDNA) from treated cells/tissue, locus-specific PCR primers with adapters, high-fidelity DNA polymerase, NGS library preparation kit, sequencer. Procedure:
- Isolate gDNA from your sample using a column-based or magnetic bead-based method.
- Amplify Target Locus using a two-step PCR approach.
- Primary PCR: Amplify the target region (200-300 bp flanking the edit site) with gene-specific primers containing partial adapter overhangs. Cycle conditions: 98°C 30s; 35 cycles of (98°C 10s, 65°C 20s, 72°C 20s); 72°C 2min.
- Indexing PCR: Add full Illumina-compatible adapters and sample indices. Cycle conditions: 98°C 30s; 8 cycles of (98°C 10s, 65°C 20s, 72°C 20s); 72°C 2min.
- Purify Amplicons using double-sided size selection magnetic beads (e.g., 0.55x / 0.85x ratios).
- Quantify & Pool Libraries using a fluorometric assay. Pool libraries equimolarly.
- Sequence on a MiSeq or equivalent platform with ≥2x250bp paired-end reads to ensure coverage across the target window.
- Analyze Data: Align reads to reference genome (e.g., with BWA). Use tools like CRISPResso2 or custom scripts to quantify the percentage of reads with intended base conversion, other nucleotide changes, and indels.
Protocol 2: Allele-Specific ddPCR for Targeted Edit Quantification Objective: To obtain absolute quantification of the frequency of a specific base edit within a bulk population. Materials: gDNA, ddPCR Supermix for Probes (no dUTP), allele-specific FAM and HEX/VIC probes (wild-type and edited), droplet generator and reader. Procedure:
- Design Probes: Design two TaqMan probes for the identical position: one complementary to the wild-type sequence (HEX/VIC), one complementary to the edited sequence (FAM). Ensure matching melting temperatures.
- Prepare Reaction Mix: For each sample, combine: 11μL ddPCR Supermix, 1.1μL each primer (900nM final), 0.6μL each probe (250nM final), 20-100ng of gDNA, nuclease-free water to 22μL.
- Generate Droplets: Transfer 20μL of mix to a DG8 cartridge. Add 70μL of Droplet Generation Oil. Generate droplets using the droplet generator.
- PCR Amplification: Transfer 40μL of emulsified droplets to a 96-well PCR plate. Seal and run: 95°C 10min; 40 cycles of (94°C 30s, 60°C 1min); 98°C 10min; 4°C hold. Use a ramp rate of 2°C/s.
- Read Droplets: Place plate in droplet reader. Analyze using QuantaSoft software.
- Calculate: Edit frequency (%) = (FAM-positive droplets / (FAM-positive + HEX-positive droplets)) * 100. Use Poisson correction for absolute copy number.
Protocol 3: Functional Readout via Restored Protein Expression (e.g., by Flow Cytometry) Objective: To measure the phenotypic correction resulting from a therapeutic base edit. Materials: Single-cell suspension from treated tissue or cells, fixation/permeabilization buffer, fluorescent-conjugated primary antibody against target protein, flow cytometry staining buffer, flow cytometer. Procedure:
- Harvest Cells: For in vivo studies, prepare a single-cell suspension from the target organ (e.g., liver via perfusion and dissociation).
- Fix and Permeabilize: Resuspend cell pellet in 4% paraformaldehyde for 15min at RT. Wash twice. Resuspend in ice-cold 90% methanol for 30min on ice to permeabilize.
- Stain for Intracellular Protein: Wash cells twice in staining buffer (PBS + 2% FBS). Resuspend in 100μL buffer containing the fluorophore-conjugated antibody at manufacturer's recommended dilution. Incubate for 1h at RT in the dark.
- Wash and Resuspend: Wash cells twice, resuspend in 200-500μL staining buffer. Pass through a 35μm strainer.
- Acquire on Flow Cytometer: Use an appropriate flow cytometer. Establish gates using unstained and isotype control samples from untreated controls.
- Analyze: The percentage of protein-positive cells and mean fluorescence intensity (MFI) indicate the level of functional restoration.
Quantitative Data Summary
Table 1: Comparison of Key Assay Parameters
| Parameter | NGS | Digital PCR | Functional Readout |
|---|---|---|---|
| Primary Output | Sequence reads; variant frequencies | Absolute copy number; % allele | % Positive cells; MFI |
| Detection Limit | ~0.1-1% | ~0.001-0.01% | Varies (often 1-5%) |
| Multiplex Capability | Very High | Moderate (2-4 plex) | High (8+ parameters) |
| Throughput | High | Medium | Medium to High |
| Key Strength | Unbiased, detects all outcomes | Sensitive, absolute quantification | Measures biological consequence |
| Limitation | Cost, complex data analysis | Only probes for known sequences | Requires specific reagent |
Table 2: Typical Outcome Metrics from an AAV-Base Editor Study in Mouse Liver
| Assay | Measurement | AAV Low Dose | AAV High Dose | Untreated Control |
|---|---|---|---|---|
| ddPCR | % Target Base Edit | 5.2% ± 0.8 | 38.5% ± 4.2 | 0.01% ± 0.005 |
| NGS (Target Locus) | % Intended Edit (Purity) | 4.8% (92%) | 35.1% (91%) | <0.01% |
| % Major Bystander Edit | 0.4% | 3.2% | 0% | |
| % Indels | 0.03% | 0.25% | 0.02% | |
| Flow Cytometry | % Protein-Positive Cells | 4.1% ± 0.9 | 32.0% ± 5.1 | 0.1% ± 0.05 |
| Mean Fluorescence Intensity (MFI) | 1,850 | 15,200 | 310 |
Diagrams
Title: Targeted NGS Analysis Workflow
Title: ddPCR Partitioning and Detection Principle
Title: Assay Correlation with Biological Cascade
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Reagents for Editing Outcome Analysis
| Item | Function & Application |
|---|---|
| High-Fidelity DNA Polymerase | Ensures accurate amplification of target locus for NGS with minimal PCR errors. |
| Droplet Digital PCR Supermix | Optimized chemical environment for precise, absolute quantification in droplet partitions. |
| Allele-Specific TaqMan Probes | Fluorescently labeled probes that differentially bind wild-type vs. edited sequences for dPCR. |
| Next-Gen Sequencing Library Kit | Facilitates the attachment of sequencing adapters and indices to amplicon libraries. |
| Magnetic Beads (Size Selection) | For purification and size-based selection of NGS amplicons to remove primer dimers. |
| Fixation/Permeabilization Kit | Prepares cells for intracellular staining to detect restored protein via flow cytometry. |
| Fluorophore-Conjugated Antibody | Enables detection and quantification of target protein expression in single cells. |
| Genomic DNA Isolation Kit | Provides high-quality, high-molecular-weight gDNA from cells or tissues for all assays. |
| CRISPResso2 Software | Standardized computational tool for quantifying genome editing outcomes from NGS data. |
Application Notes
The selection of an optimal adeno-associated virus (AAV) serotype is a critical, foundational step in the development of gene therapies, particularly for delivery of base editors in a therapeutic thesis. This choice involves a fundamental trade-off between transduction efficiency (potency) and safety profile (including immunogenicity, off-target tropism, and cellular toxicity). The ideal serotype maximizes delivery to the target tissue while minimizing pre-existing neutralizing antibodies, unintended biodistribution, and dose-dependent toxicities.
Recent data from preclinical studies in non-human primates (NHPs) and human clinical trials highlight serotype-specific profiles. For instance, while AAV9 and AAVrh.10 are highly efficient for crossing the blood-brain barrier and targeting the central nervous system (CNS), they also exhibit widespread biodistribution to the liver, a key organ for toxicity. Conversely, engineered capsids like AAV-PHP.eB show enhanced CNS tropism in specific mouse models but may not translate directly to humans. For muscle targets, AAV8 and AAV9 are highly efficient, but AAV8 shows higher liver sequestration. In retinal gene therapy, AAV2 and its variants (e.g., AAV2-7m8) remain staples due to localized delivery, but immunogenicity remains a concern.
Safety is profoundly influenced by total viral genome load, with high doses correlating with hepatotoxicity and thrombotic microangiopathy in systemic deliveries. The presence of pre-existing neutralizing antibodies (NAbs) against common serotypes like AAV1, AAV2, AAV8, and AAV9 in a significant portion of the population can abrogate efficacy. Therefore, serotype selection must be guided by patient stratification (NAb screening) and a detailed understanding of the efficiency-safety balance for the intended tissue.
Data Tables
Table 1: Key AAV Serotype Tropism and Efficiency Metrics
| Serotype | Primary Tissue Targets (High Efficiency) | Key Strengths | Key Limitations (Safety/Efficiency) |
|---|---|---|---|
| AAV1 | Skeletal Muscle, Heart | High muscle transduction, lower liver tropism vs AAV8/9 | Moderate pre-existing immunity in humans. |
| AAV2 | Liver, Retina, CNS (with direct injection) | Well-characterized, stable transduction. | Very high pre-existing NAb prevalence; requires high MOI. |
| AAV5 | CNS, Retina, Synovium | Low cross-reactivity with anti-AAV2 NAbs. | Moderate overall transduction efficiency in many tissues. |
| AAV8 | Liver, Pancreas, Muscle | Superior hepatocyte transduction (mice/NHPs). | High liver sequestration for non-liver targets; common NAb presence. |
| AAV9 | CNS, Heart, Muscle, Liver | Crosses BBB in mice/NHPs; broad tropism. | Very broad biodistribution (safety concern); high NAb prevalence. |
| AAV-DJ | Liver, Retina, Muscle | Hybrid; high in vitro infectivity across cell types. | Complex immunogenicity profile, off-target effects. |
| AAVrh.10 | CNS, Retina | Efficient CNS transduction, alternative to AAV9. | Similar broad biodistribution as AAV9. |
| AAV-PHP.eB | CNS (in specific mouse models) | Dramatically enhanced CNS transduction after IV delivery in mice. | Activity dependent on mouse Ly6a; not effective in NHPs/humans. |
Table 2: Safety and Immunogenicity Profiles
| Serotype | Approx. Human NAb Seroprevalence (%) | Notable Clinical Safety Concerns (Systemic Delivery) | Dose-Limiting Toxicity (Primary Organ) |
|---|---|---|---|
| AAV2 | 30-70% | High immunogenicity, T-cell responses against transgene. | Liver (at high dose). |
| AAV8 | ~30-40% | Thrombotic microangiopathy, hepatotoxicity. | Liver, endothelium. |
| AAV9 | ~30-50% | Hepatotoxicity, cardiotoxicity, dorsal root ganglion pathology. | Liver, Heart. |
| AAVrh.10 | ~20-30%* | Similar to AAV9; long-term monitoring ongoing. | Liver, CNS (potential). |
*Estimated based on cross-reactivity studies.
Experimental Protocols
Protocol 1: In Vivo Biodistribution and Efficiency Comparison Objective: Quantify viral genome copy numbers and transgene expression across tissues following systemic administration of different AAV serotypes carrying a base editor construct.
- Vector Preparation: Purify AAV vectors (serotypes 1, 8, 9, rh.10) encoding a GFP-tagged base editor via iodixanol gradient ultracentrifugation. Titrate via ddPCR.
- Animal Dosing: Inject 6-week-old C57BL/6 mice (n=5/group) intravenously via tail vein with 1x10^11 vg of each AAV preparation in 100 µL PBS. Include a PBS control group.
- Tissue Harvest: At 4 weeks post-injection, euthanize mice. Collect and weigh tissues: brain, heart, liver, lung, skeletal muscle, kidney, and spleen.
- DNA/RNA Extraction: Homogenize tissues. Use a kit to isolate genomic DNA and total RNA from aliquots of homogenate.
- Biodistribution (qPCR/ddPCR): Perform ddPCR on gDNA using primers/probe against the viral polyA sequence to determine vector genome copies per µg DNA.
- Efficiency Assessment (RT-qPCR): Reverse transcribe RNA to cDNA. Perform RT-qPCR for GFP mRNA expression, normalized to Gapdh.
- Analysis: Calculate vg/diploid genome and relative mRNA expression. Compare across serotypes and tissues.
Protocol 2: In Vitro Neutralizing Antibody (NAb) Assay Objective: Determine the titer of serum NAbs against various AAV serotypes to inform serotype selection for clinical translation.
- Serum Collection: Heat-inactivate test sera (human or NHP) at 56°C for 30 min. Perform serial 2-fold dilutions in culture medium.
- Virus-Antibody Incubation: Mix a fixed dose of AAV-GFP (MOI ~10^4) of each serotype with an equal volume of diluted serum. Incubate at 37°C for 1 hr.
- Cell Infection: Add mixtures to HEK293 cells in a 96-well plate. Include virus-only (no serum) and cell-only controls.
- Flow Cytometry: At 48 hours post-transduction, harvest cells and analyze the percentage of GFP-positive cells via flow cytometry.
- Titer Calculation: The NAb titer is defined as the highest serum dilution that reduces transduction efficiency by ≥50% (IC50) compared to the virus-only control.
Diagrams
Diagram 1: AAV Serotype Selection Workflow for Base Editor Research
Diagram 2: AAV Serotype Tropism by Target Tissue
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function/Description |
|---|---|
| AAV Purification Kits (Iodixanol) | For laboratory-scale, high-purity AAV vector preparation via ultracentrifugation. |
| ddPCR Supermix for AAV Quantification | Provides absolute quantification of vector genome titer without a standard curve, essential for accurate dosing. |
| Neutralizing Antibody Assay Kit | Standardized in vitro kit for detecting NAbs against multiple AAV serotypes in serum/plasma. |
| Tissue DNA/RNA Co-isolation Kit | Enables simultaneous extraction of gDNA (for biodistribution) and RNA (for expression) from the same tissue sample. |
| High-Sensitivity NGS Base Editing Analysis Service | Provides deep sequencing and unbiased analysis of on-target editing and genome-wide off-target effects. |
| Pre-Packaged AAV Serotype Library | A set of isogenic AAV vectors differing only in capsid serotype, enabling controlled comparative studies. |
| Recombinant Ancestral AAV (AncAAV) Capsids | Engineered capsids with enhanced thermostability and potentially lower immunogenicity for research use. |
This application note is framed within a broader thesis on AAV delivery for base editing research, aiming to provide a practical, data-driven comparison of three primary in vivo delivery modalities: Adeno-Associated Virus (AAV), Lipid Nanoparticles (LNPs), and Extracellular Vesicles (EVs). The focus is on their application for delivering base editor ribonucleoproteins (RNPs) or mRNA/DNA payloads to target tissues for precise genome editing.
Table 1: SWOT Analysis of Base Editor Delivery Modalities
| Aspect | AAV-Base Editors | LNP-Base Editors | EV-Base Editors |
|---|---|---|---|
| Strengths | • High transduction efficiency in vivo• Long-term expression in non-dividing cells• Well-established clinical safety profile | • High payload capacity• Transient expression reduces off-target risk• Scalable, modular manufacturing | • Native biocompatibility & low immunogenicity• Potential for natural tissue tropism• Can bypass some biological barriers |
| Weaknesses | • Limited cargo capacity (~4.7kb)• Pre-existing immunity in population• Risk of genomic integration (rare) | • Potential systemic toxicity (ionizable lipids)• Rapid clearance by MPS• Liver-dominant tropism can be a limitation | • Complex isolation & standardization• Low yield & heterogeneous composition• Limited engineering control over cargo loading |
| Opportunities | • Engineering of novel synthetic capsids for improved tropism• Dual-vector split systems to overcome size limits | • Combinatorial library screening for novel tissue-specific ionizable lipids• Co-delivery of multiple editor mRNAs/sgRNAs | • Engineering as "designer exosomes"• Exploiting endogenous homing mechanisms for targeted delivery |
| Threats | • Immune response eliminating transduced cells• Anti-capsid antibodies neutralizing delivery• High cost of GMP manufacturing | • Dominant patents may limit access• Potential for accelerated blood clearance (ABC) phenomenon with repeat dosing | • Regulatory uncertainty for EV-based therapeutics• Competition from more engineered synthetic platforms |
Table 2: Quantitative Performance Comparison (Recent Preclinical Data)
| Parameter | AAV | LNP | EV |
|---|---|---|---|
| Typical Editing Efficiency in vivo (Liver) | 20-60% (stable) | 40-80% (transient peak) | 5-25% (reported range) |
| Onset of Expression | Days to weeks | Hours to days | Hours to days |
| Duration of Expression | Months to years | Days to a week | Days |
| Dose for Liver Editing (mouse) | 1e11 - 1e13 vg/mouse | 0.5 - 1.0 mg/kg mRNA | 1e10 - 1e11 particles/mouse |
| Immunogenicity Risk | Moderate-High (cellular & humoral) | Moderate (mainly humoral to PEG) | Low-Moderate |
Detailed Protocols
Protocol 3.1: AAV Production & Purification for Base Editor Delivery (Triple Transfection in HEK293T)
Application: Production of research-grade AAV serotype(s) (e.g., AAV9, AAV-LK03, PHP.eB) encoding a base editor (ABE or CBE) and sgRNA expression cassette. Materials:
- HEK293T cells at 70-80% confluency in 10-layer CellSTACKs.
- Polyethylenimine (PEI) Max, 1 mg/mL.
- Plasmid Triad: pAAV-BE (ITR-flanked editor), pAAV-RC (Rep/Cap for serotype), pHelper (Adenoviral genes).
- Benzonase (for digesting unpackaged nucleic acids).
- Iodixanol Gradient Solutions (15%, 25%, 40%, 60% in PBS-MK).
- Dulbecco's Modified Eagle Medium (DMEM) with 10% FBS. Procedure:
- Transfection: For one CellSTACK, mix 150 µg each of the three plasmids in 30 mL serum-free DMEM. Add 1.2 mL PEI Max, vortex, incubate 15 min at RT. Add dropwise to cells in fresh medium.
- Harvest: At 72h post-transfection, collect cells and media. Pellet cells via centrifugation (2000 x g, 20 min). Resuspend cell pellet in lysis buffer (150 mM NaCl, 50 mM Tris-HCl, pH 8.5) and perform three freeze-thaw cycles.
- Benzonase Treatment: Add Benzonase (50 U/mL) to lysate and supernatant, incubate at 37°C for 30 min.
- Iodixanol Gradient Ultracentrifugation: Layer clarified lysate onto a pre-formed iodixanol step gradient (15%, 25%, 40%, 60%) in a quick-seal tube. Ultracentrifuge at 350,000 x g, 2.5h, 18°C in a fixed-angle rotor (e.g., Type 70 Ti).
- Collection & Dialysis: Extract the opaque 40% iodixanol fraction. Dialyze against PBS-MK (PBS with 1 mM MgCl2, 2.5 mM KCl) overnight at 4°C. Aliquot and titer via qPCR (ITR-specific primers).
Protocol 3.2: Formulation of LNPs for Base Editor mRNA/sgRNA Co-Delivery
Application: Formulation of ionizable lipid-based LNPs encapsulating base editor mRNA and chemically modified sgRNA. Materials:
- Lipids in Ethanol: Ionizable lipid (e.g., DLin-MC3-DMA, SM-102), DSPC, Cholesterol, DMG-PEG2000.
- Aqueous Phase: Base editor mRNA and sgRNA in citrate buffer (pH 4.0).
- Microfluidic Mixer (e.g., NanoAssemblr Ignite).
- Tangential Flow Filtration (TFF) system with 100 kDa MWCO membranes. Procedure:
- Prepare Lipid Stock: Mix ionizable lipid, DSPC, cholesterol, and DMG-PEG2000 at a molar ratio of 50:10:38.5:1.5 in ethanol to a total lipid concentration of 12.5 mM.
- Prepare Aqueous RNA Stock: Combine base editor mRNA and sgRNA at a molar ratio of 1:3 in 50 mM citrate buffer, pH 4.0. Final RNA concentration should be 0.2 mg/mL.
- Microfluidic Mixing: Using the microfluidic instrument, set the total flow rate (TFR) to 12 mL/min and a flow rate ratio (FRR) of 3:1 (aqueous:ethanol). Simultaneously pump the RNA solution and lipid solution into the mixing chamber.
- Buffer Exchange & Concentration: Immediately dilute the formed LNP mixture with 4 volumes of PBS (pH 7.4). Concentrate and diafilter against PBS using TFF.
- Sterile Filtration & Characterization: Filter through a 0.22 µm PES membrane. Characterize particle size (expected 70-100 nm via DLS), PDI (<0.2), encapsulation efficiency (>90% via RiboGreen assay), and endotoxin levels.
Protocol 3.3: Isolation & Cargo Loading of EVs for Base Editor RNP Delivery
Application: Isolation of exosomes from mesenchymal stem cell (MSC) conditioned media and loading with base editor RNPs via sonication. Materials:
- Serum-free MSC Conditioned Media (collected over 48h).
- Total Exosome Isolation (from media) Kit or differential centrifugation reagents.
- Base Editor RNP: Pre-complexed Alt-R S.p. HiFi Cas9 Nickase-BE3 protein with synthetic sgRNA.
- Sonication Probe and water bath.
- Phosphate-Buffered Saline (PBS), sterile-filtered.
- qNano Gold Instrument with NP200 nanopores for sizing. Procedure:
- EV Isolation: Centrifuge conditioned media at 2,000 x g for 30 min to remove cells. Filter supernatant through a 0.22 µm filter. Add 0.5 volumes of isolation reagent, incubate overnight at 4°C. Centrifuge at 10,000 x g for 1h at 4°C. Resuspend EV pellet in sterile PBS.
- RNP Loading via Sonication: Mix 1x10^10 EV particles (quantified by NTA) with 10 µg of pre-complexed base editor RNP in 500 µL PBS. Place on ice. Sonicate using a probe sonicator at 20% amplitude for six cycles of 30 sec pulse/30 sec rest, keeping the sample on ice.
- Purification: Remove unloaded RNP by ultracentrifugation at 100,000 x g for 70 min at 4°C. Wash pellet once in PBS and resuspend in 100 µL PBS.
- Characterization: Analyze size distribution and concentration via nanoparticle tracking analysis (NTA). Confirm RNP loading via western blot for the base editor protein or a fluorophore-labeled sgRNA assay.
Visualizations
Diagram 1: AAV-Base Editor In Vivo Delivery Pathway
Diagram 2: Base Editor Delivery Modality Selection Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Base Editor Delivery Research
| Reagent / Material | Provider Examples | Function in Research |
|---|---|---|
| AAV Serotype-Specific Rep/Cap Plasmids | Addgene, Vigene | Provides the viral capsid proteins determining tissue tropism for AAV production. |
| Ionizable Lipids (e.g., SM-102, ALC-0315) | MedChemExpress, Avanti | Key component of LNPs for efficient mRNA encapsulation and endosomal escape. |
| Base Editor mRNA (5-moU modified) | TriLink BioTechnologies | The transient payload for LNP delivery, encoding the base editor protein. High purity and capping critical. |
| Chemically Modified sgRNA (2'-O-methyl, phosphorothioate) | IDT, Synthego | Enhances stability and reduces immunogenicity of the guide RNA across all delivery platforms. |
| Exosome Isolation Kits (CD63/CD81 magnetic beads) | System Biosciences, Thermo Fisher | For rapid pull-down and characterization of EVs from cell culture media or biofluids. |
| Anti-AAV Neutralizing Antibody Assay Kits | Progen, Spark Therapeutics | Quantifies pre-existing humoral immunity against specific AAV serotypes in animal or human sera. |
| Next-Generation Sequencing Kits for Off-Target Analysis (e.g., GUIDE-seq, ONE-seq) | Integrated DNA Technologies | Essential for quantifying on-target editing efficiency and genome-wide off-target effects across modalities. |
| PBS-MK Buffer | Made in-house or custom | Standard dialysis and formulation buffer for AAV, preserving viral particle stability and infectivity. |
| RiboGreen Assay Kit | Thermo Fisher | Quantifies both encapsulated and free RNA in LNP formulations to determine loading efficiency. |
| Recombinant Base Editor Protein (e.g., BE4max, ABE8e) | Aldevron, Thermo Fisher | Critical for generating RNPs for direct delivery or EV loading experiments. |
Within the broader thesis on AAV delivery for base editors, the transition from preclinical research to early-phase clinical trials is critical. This section reviews recent clinical data and the evolving regulatory framework, focusing on safety, proof-of-concept, and the unique considerations for AAV-base editor therapies.
Current Early-Phase Clinical Trial Landscape for AAV-Gene Editing Therapies
Recent trials provide initial safety and biodistribution data. Key quantitative findings from published early-phase (I/II) trials are summarized below.
Table 1: Summary of Select Early-Phase Clinical Trials Involving AAV-Delivered Gene Editors (as of 2024)
| Therapeutic Target / Condition | Delivery Vector | Editor Type | Phase | Primary Outcomes (Safety & Efficacy) | Key Reference / Identifier |
|---|---|---|---|---|---|
| Leber Congenital Amaurosis 10 (CEP290) | AAV5 | CRISPR-Cas9 (Nuclease) | I/II (BRILLIANCE) | Generally tolerable; modest visual improvements in some patients. | NCT03872479 |
| Transthyretin Amyloidosis (ATTR) | AAV8 | CRISPR-Cas9 (Nuclease) | I | Dose-dependent serum TTR reduction; adverse events included infusion reactions. | NCT04601051 |
| Glycogen Storage Disease Ia (GSDIa) | AAV8 | Base Editor (ABE) | I/II (Pre-Clinical to Clinical Transition) | Preclinical data showed metabolic correction; clinical safety pending. | Preclinical Lead |
| Huntington's Disease | AAV9 | Zinc Finger Transcriptional Repressor | I/II | Well-tolerated; dose-dependent reduction of mutant huntingtin protein in CSF. | NCT05111249 |
| Hemophilia B | AAV8 | - | I/II (Gene Addition) | Established safety profile for AAV8-FIX; informs vector immunology for editor delivery. | NCT00979238 |
Critical Data Review and Analysis Protocols
Protocol for Integrated Safety and Biodistribution Analysis from Clinical Samples
Objective: To comprehensively assess the safety profile and vector/editor biodistribution in early-phase trial participants. Materials:
- Patient serum/plasma, PBMCs, CSF, and tissue biopsies (as applicable).
- ddPCR/qPCR systems, NGS platform, ELISA/MSD assays, clinical chemistry analyzers. Methodology:
- Sample Collection: Serial samples collected pre-dose and at defined intervals post-vector administration.
- Vector Genome Biodistribution (qPCR/ddPCR):
- Extract total DNA from samples using a column-based kit.
- Perform absolute quantification using vector-specific primers/probe (e.g., targeting the polyA signal). Report as vg/µg genomic DNA or vg/mL fluid.
- Off-Target Analysis (NGS):
- Perform whole-genome sequencing (WGS) on pre- and post-treatment PBMC DNA.
- Use in silico predicted off-target sites and unbiased methods (e.g., GUIDE-seq, CIRCLE-seq) adapted for base editors to identify sequencing regions.
- Align sequences and call variants using a pipeline (e.g., GATK). Filter against pre-treatment background.
- Immunogenicity Assessment:
- Anti-AAV Capsid Antibodies: Measure via ELISA using empty AAV capsids.
- Anti-Editor Antibodies: Use an immunoassay with recombinant editor protein.
- Cellular Immune Responses: Perform IFN-γ ELISpot on PBMCs stimulated with capsid or editor peptides.
- Clinical Safety Monitoring: Record all adverse events, graded by CTCAE v6.0. Monitor liver function (ALT, AST), complement activation, and platelet counts.
Protocol for Evaluating Proof-of-Biological-Activity
Objective: To measure the intended molecular editing effect and functional outcome. Materials: Target tissue biopsies, cDNA synthesis kit, NGS reagents, functional assay reagents (e.g., substrate for an enzyme). Methodology:
- Target Site Editing Efficiency (NGS):
- Amplify the genomic target region from tissue DNA using PCR.
- Prepare NGS libraries and sequence at high depth (>100,000x).
- Analyze base conversion percentages at the target locus using computational tools (e.g., CRISPResso2 for base editors).
- Functional Restoration:
- For metabolic diseases, measure enzyme activity in tissue lysates using a fluorogenic or chromogenic substrate.
- For dominant disorders, quantify mutant protein reduction via immunoassay (e.g., Simoa).
- Correlate biochemical correction with editing efficiency.
Regulatory Considerations & Development Pathway
Navigating the regulatory path for an AAV-delivered base editor requires early and frequent engagement.
- Pre-IND Meeting: Critical to align on CMC, toxicology study design (relevant animal model, dosing regimen), and proposed clinical endpoints.
- Chemistry, Manufacturing, and Controls (CMC): Expect heightened scrutiny on vector and editor purity, potency assays (in vitro editing efficiency), and characterization of impurities (e.g., residual DNA from producer cells).
- Nonclinical Toxicology: Requirements include biodistribution, integration/seeding studies, germline transmission risk assessment, and off-target editing analysis in relevant tissues.
- Clinical Trial Design: First-in-Human (FIH) trials typically adopt a single-ascending dose (SAD) design. Key considerations include:
- Starting dose justification (based on MABEL - Minimum Anticipated Biological Effect Level).
- Patient population (severely affected vs. earlier intervention).
- Monitoring for delayed adverse events (e.g., genotoxicity, immune responses).
- Long-Term Follow-Up: Regulatory mandates (e.g., FDA guidance requires 15-year follow-up for gene therapy) to monitor persistence and long-term safety.
Visual Summaries
Title: AAV Base Editor Clinical Development Pathway
Title: Clinical Sample Analysis & Decision Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents & Tools for AAV-Base Editor Clinical Trial Analysis
| Item | Function & Application in Clinical Trial Context |
|---|---|
| AAV Serotype-Specific ELISA Kits | Quantify anti-AAV neutralizing antibodies in patient serum prior to dosing to determine eligibility. |
| ddPCR Supermix for Absolute Quantification | Precisely measure vector genome copies in patient tissue biopsies and bodily fluids (vg/µg DNA). |
| Hybridization-Based NGS Capture Panels | Designed for targeted deep sequencing of the genomic locus and in silico predicted off-target sites from PBMC/tissue DNA. |
| CRISPResso2 or BE-Analyzer Software | Computational pipeline to quantify base editing efficiency and outcome percentages from NGS data. |
| Recombinant Editor Protein & Peptide Pools | Used as antigens in immunoassays to detect and monitor cellular (ELISpot) and humoral (ELISA) immune responses against the base editor. |
| Ultra-Sensitive Immunoassay Platform (e.g., Simoa) | Detect low-abundance biomarkers (e.g., mutant protein reduction, GFAP for neuroinflammation) in patient CSF or serum. |
| Next-Gen Sequencing Standards (Horizon Discovery, etc.) | Validated reference cell lines with known edits for calibrating NGS-based off-target analysis pipelines. |
| GMP-Grade AAV Reference Standard | Critical for validating potency assays and ensuring consistency in vector genome quantification across trial sites. |
Conclusion
AAV delivery represents a powerful and clinically validated modality for in vivo base editing, offering the potential for durable, single-administration therapies for genetic disorders. Success hinges on a balanced integration of foundational virology, precise molecular tool engineering, and rigorous preclinical optimization to address packaging limits, specificity, and immune evasion. While dual-vector systems and novel capsids are overcoming early size constraints, the comparative landscape shows AAVs leading in persistent expression for post-mitotic tissues. Future directions must prioritize the development of more compact, high-specificity editors, refined immune modulation strategies, and scalable manufacturing. As clinical trials progress, the convergence of optimized AAV vectors with next-generation base editors promises to redefine the therapeutic paradigm for precise genomic medicine.